Hip dysplasia, or developmental dysplasia of the hip (DDH), is a congenital musculoskeletal condition in which the acetabulum (hip socket) is too shallow to securely hold the femoral head. This structural abnormality can result in instability, partial or full dislocation, and break down of cartilage. If this is undiagnosed in childhood, many individuals begin to experience symptoms such as pain, stiffness, and reduced range of motion in early adulthood.
Addressing the functional seating needs of clients with hip dysplasia is essential to promote independence, reduce pain, and prevent secondary complications such as joint degeneration, postural deformities, and reduced participation in daily activities.
Jump straight to…
Why Seating is Important for Hip Dysplasia
Seating plays a critical role in:
- Supporting appropriate postural alignment
- Reducing compensatory movement patterns
- Facilitating safe transfers and mobility
- Enhancing participation in meaningful activities
Clients with symptomatic hip dysplasia often present with pain during prolonged sitting, difficulty maintaining neutral pelvic alignment, and challenges with sit-to-stand transitions. Appropriate seating solutions must be adaptable to individual functional goals and living environments.
Key Features of Suitable Seating for Hip Dysplasia
When prescribing seating for clients with hip dysplasia, the following features should be considered.
Adjustable Seat Height
Clients should have hips positioned slightly higher than the knees to reduce flexion strain. Chairs with adjustable height mechanisms can support this.
High-Density Foam Cushions
Firm seat cushions prevent excessive sinking, maintain joint alignment, and distribute pressure more evenly.
Contoured Backrests
Contoured backrests promote upright posture and reduce compensatory pelvic tilt.
Tilt-in-Space or Recline Options
Tilt in space is useful for clients with coexisting conditions or those requiring pressure relief and hip unloading.
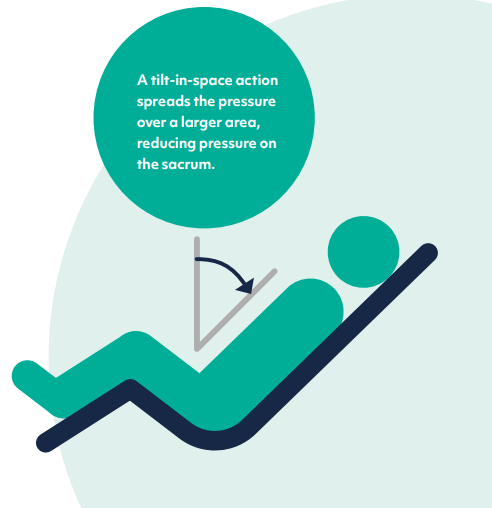
Tilt-in-space functionality
Stable Armrests
Stable armrests facilitate upper-body support and safe transfers.
Seat Width and Depth
Adequate space avoids forced adduction or rotation; consider abduction blocks or positioning wedges where needed.
Transfer Compatibility
Chairs must be compatible with hoists, stand aids, or other mobility equipment when used in care home settings.
Recommended Chair Types
Postural Management Seating
Designed for clinical use, care chairs like the Lento Care Chair offer extensive adjustability, pressure management, and optional accessories like lateral supports or pommels. These are ideal for clients with complex needs in care home or rehab settings.
Rise and Recline Chairs
Rise and recline chairs allow a graded recline and assist with transfers. For clients with reduced lower limb strength, these promotes safety and autonomy.

Ergonomic Task Chairs
For clients living independently or those working in seated environments, task chairs like the VELA Activity chair offer custom positioning, pelvic tilt control, and active sitting features.
Saddle Chairs
For short duration tasks, saddle stools promote a neutral pelvic tilt and reduced hip flexion. They are best for clients with adequate trunk control performing tasks at a work counter.
Modular Shower and Commode Seating
For hygiene routines, consider modular tilt-in-space shower chairs with pressure-relieving cushions and adjustable seat angles.
Seating Prescriptions for Hip Dysplasia
When assessing seating for hip dysplasia, complete a full postural and functional assessment, including hip range of movement, pain levels, transfer ability, and cognition. Also consider any coexisting diagnoses, such as spinal deformities, arthritis, or neurological conditions.
Use clinical reasoning to justify any deviation from standard seating—e.g., abduction bracing, asymmetrical cushions.
Monitor seating effectiveness regularly and review in line with changes in function, pain, or weight.
Sitting Techniques to Train Clients with Hip Dysplasia
In addition to clinical seating, clients with hip dysplasia can benefit from training with sitting techniques.
Neutral pelvic alignment
Use tactile cues, mirrors, or proprioceptive feedback to promote correct posture.
Use of assistive cushions
Wedge or coccyx cushions can support joint alignment and reduce pressure.
Avoidance of cross-legged sitting
Reinforce hip-safe postures that avoid internal rotation.
Active movement breaks
Encourage weight shifts and micro-breaks every 30 – 60 minutes for ambulant clients.
Safe transfer practice
Incorporate chair height and armrest use into transfer retraining sessions.
Frequently Asked Questions
How does hip dysplasia affect sitting tolerance?
Clients often experience increased pain and fatigue when seated due to joint instability and compression. Improper support can exacerbate these symptoms.
Are standard riser recliners appropriate for care settings?
Only if they offer sufficient adjustability, support, and transfer compatibility. Always assess for appropriate height, seat firmness, and safety features.
Can cushions alone correct poor seating?
Cushions can aid alignment or comfort but must be used in combination with a clinically appropriate seating system.
How often should seating be reviewed?
At minimum every 6 – 12 months, or sooner if there are functional changes, pressure risk, or progression in joint degeneration.
Do all clients need with hip dysplasia need specialist chairs?
Not necessarily, some may do well with adapted domestic chairs, ergonomic seating, or even activity chairs, depending on their level of function and goals.
Conclusion
For OTs and physios supporting clients with hip dysplasia, seating is a cornerstone of functional rehabilitation. From positioning to participation, the right chair enables comfort, safety, and independence. A thorough assessment, evidence-based equipment selection, and client education are key to achieving optimal outcomes.
Free & No Obligation Assessment














