With seating being such a major part of life for those with mobility challenges, it can be daunting to know how to carry out an effective seating assessment.
This article is a useful guide on the steps behind an effective seating assessment, helping you formulate a process that will increase your confidence as a healthcare professional when specifying seating for your clients.
Jump straight to…
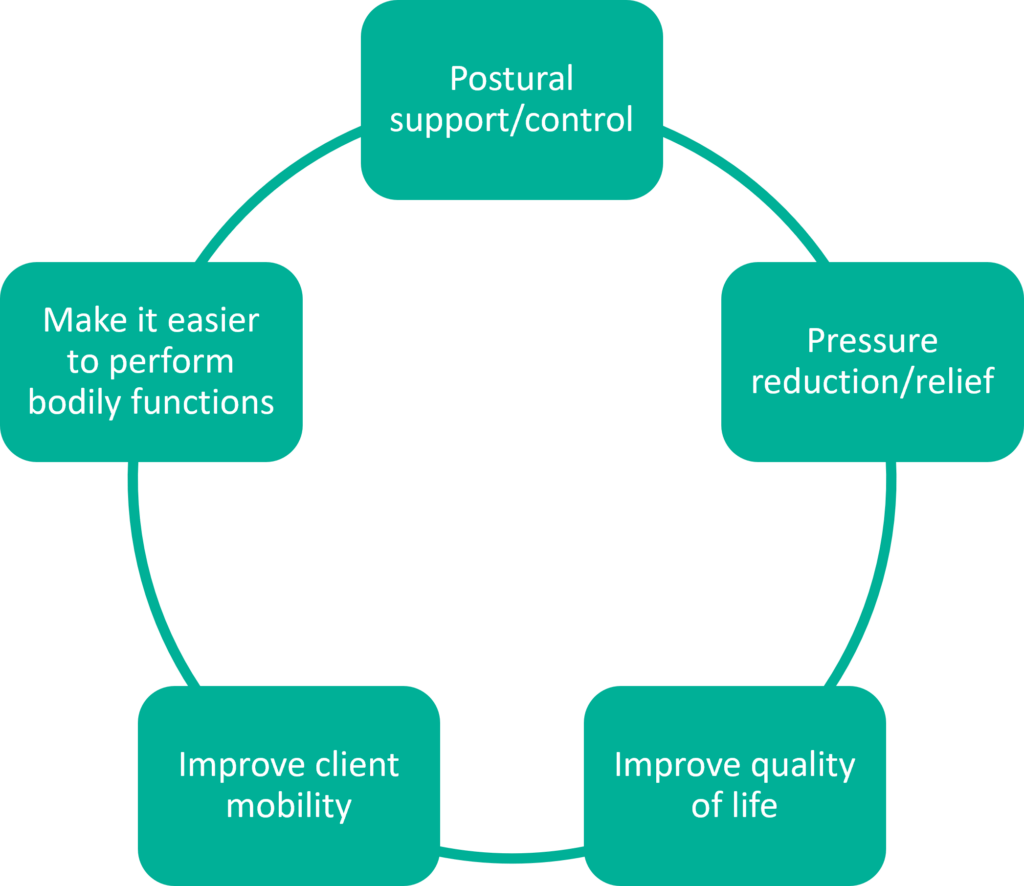
Why is Seating So Important?
For the elderly and disabled that are sitting for longer than most, there are a whole list of unpleasantries that come with incorrect seating:
- Poor posture
- Joint, muscle, back, or shoulder pain
- Irritated tissue or pressure damage
- Poor circulation
- Difficulty in getting up
- A lack of independence
- Reduced confidence, or social isolation
- Contractures and deformities
Put simply: poor seating – leads to poor posture – leads to pain and discomfort. However, the good news is that we can reverse this process by carrying out a detailed seating assessment and prescribing the correct seating.

According to Pauline Pope, this is what good posture looks like:
- It facilitates effective functional performance
- It’s energy efficient
- It does not harm the body systems.
So how do we carry out an effective seating assessment?
Beginning a Seating Assessment
When undertaking a seating assessment, the first step is to look at the client’s current situation and what goals they want to achieve with new seating. Ensure plenty of notes are taken at this stage, as these will form a foundation of your seating decisions and will be useful to refer back to in future if their seating needs change.
The Here and Now
As part of looking at the client’s current situation, consider their current seating provision – is their chair uncomfortable? How long have they been using it? Is it making their posture worse? Answering these questions will help you uncover the root causes of their current seating issues.
Postural problems – Fixed or Flexible?
When looking at how their current chair is impacting their posture, we need to decide if their posture is fixed or flexible.
A fixed postural deformity cannot be corrected, so needs to be accommodated with positioning aids that can be built into their new chair. If it is flexible, it can be corrected by specifying the right seating. This can be determined by their physical presentation in the chair, checking their pelvic position (more on this below), and lying them on a plinth to see if their posture can be straightened.
Some examples of flexible postural issues are a forward lean (kyphosis) and rounded shoulders. People adopt poor posture when using the wrong-sized chair, which leads to uneven weight distribution. However, a kyphosis could be fixed if they have a spinal deformity, so it is important to identify the causes of postural problems from the outset.
The Client’s Needs
As part of your assessment notes, take the client’s full details and notes of their medical history including any long-term conditions they have.
It is important to get a holistic view of the client’s situation, so talking to them and asking them questions about their daily routine will help you find out their hobbies and functional needs. This is all relevant to the seating assessment, as their seating will need to accommodate these daily activities.
Seating Goals
Ask the client what goals they want to achieve with new seating, whether this is getting outside, being able to socialise more with friends or family, or just live in comfort without postural pain!
In looking towards the future, we want to consider the progression of any long-term condition they might have, for example neurological conditions like MS or MND. This will help future-proof their requirements and provide the ability for their seating to be adapted in line with their condition, as their needs change over time.
Before trying the client in a chair, these are some of the factors you might want to think about (in no particular order):
- How mobile are they? How do they transfer?
- Can they sit up without support? If so, how long for?
- Can they alter their position themselves whilst sitting?
- How long will the person be sitting for?
- How comfortable can we make them? Where and how do they experience discomfort at the moment?
- Is it safe to leave them in a chair? Are they at risk of sliding out? Is it safe to let them operate the chair themselves? Can they stand unaided? Will they try to stand even if they can’t? Are there pets or children in the house?
To see the full list of factors, download The Healthcare Professional’s Complete Guide to Specialist Seating Assessments.
Meeting the Client’s Physical, Social and Emotional Needs
Seating Starts with the Pelvis
As we have said so many times, the pelvis is the foundation of good posture! It really is, and we have lots of useful resources to bring this to life for you, such as our recent webinar on this subject.
The position of the ASIS and PSIS in relation to each other is the basis of your postural assessment. To check the alignment of the client’s pelvis, feel where the client’s PSIS and ASIS points are, with their permission. In an ideal situation, the ASIS and PSIS must be level, with the pelvis tilted ever-so-slightly forwards (known as minimal anterior pelvic tilt). It’s worth mentioning that some people have a fixed deformity which makes it impossible to get complete alignment.
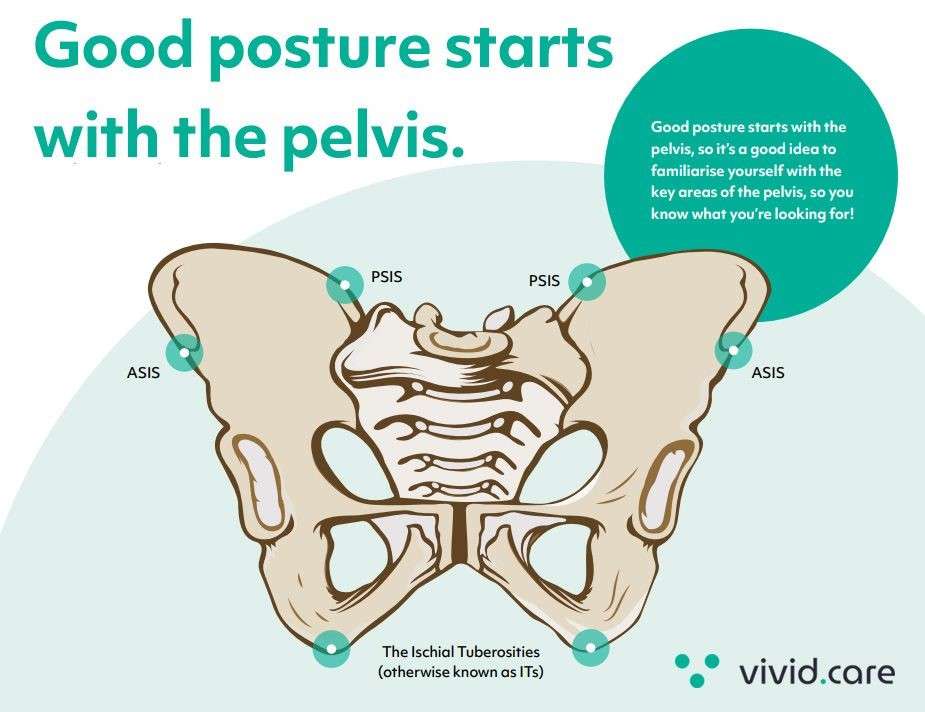
Our aim is to get their sitting posture centralised and weight evenly distributed as much as possible, and having correct pelvic alignment is at the base of this.
Common postural abnormalities
When it comes to abnormal positioning, there are lots of fancy phrases that get thrown around — I’m sure you’ll have heard of some of the conditions we mention below. However, don’t be intimidated — they aren’t as complicated as you may think.
Postural Deformity | Definition |
Posterior Tilt | The PSIS is lower than the ASIS – in other words, the pelvis is tilted backwards. This is sometimes called ‘sacral sitting’ |
Anterior Tilt | The PSIS is higher than the ASIS – opposite to
posterior tilt and not as common. |
Pelvic Obliquity | One ASIS is higher than the other, making the patient appear to be falling to one side. |
Pelvic Rotation | One ASIS is further forward than the other, which can lead to windswept hips. |
Kyphosis | A rounded curve at the top of the spine causing a ‘hunched’ posture |
Scoliosis | Sideways curve or ‘twisted’ spine, causing a C-shaped curve. |
Lordosis | An increased lumbar curve in the spine. |
We also cover other postural deformities in our Ebook like:
- Abduction and Adduction
- Contractures
- Leg Length Discrepancy
- Windswept Hip
To see even more hints and tips on how seating can help to alleviate postural conditions and abnormalities, download our Seating Assessment eBook.
Providing Comfort
The primary goal of any seating should be to provide long-term comfort for the client by promoting good posture and body alignment. This reduces the risk of developing any musculoskeletal disorders from poor posture, and alleviates joint pain or muscle stiffness.
Reducing Pressure
If you’re a healthcare professional, you’ll know that pressure care is a huge subject.
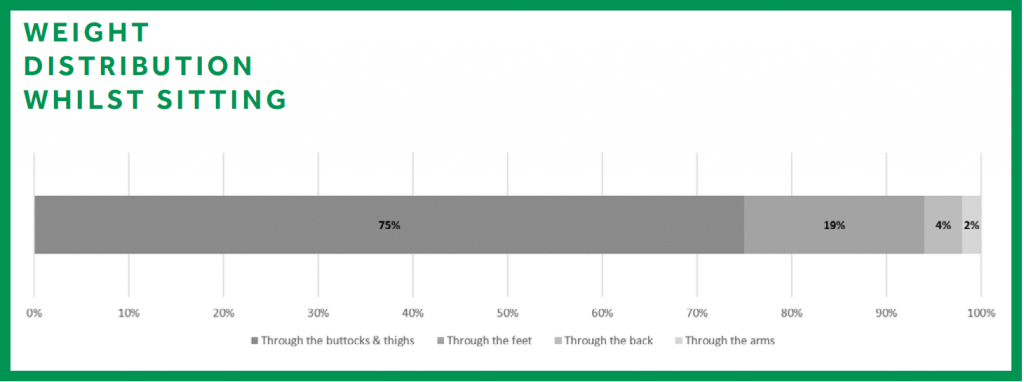
The interesting thing is, seat sizing has a huge impact on both posture and pressure care. So if you get seat sizing correct (we’ll go into this in more detail later), you’re over halfway there.
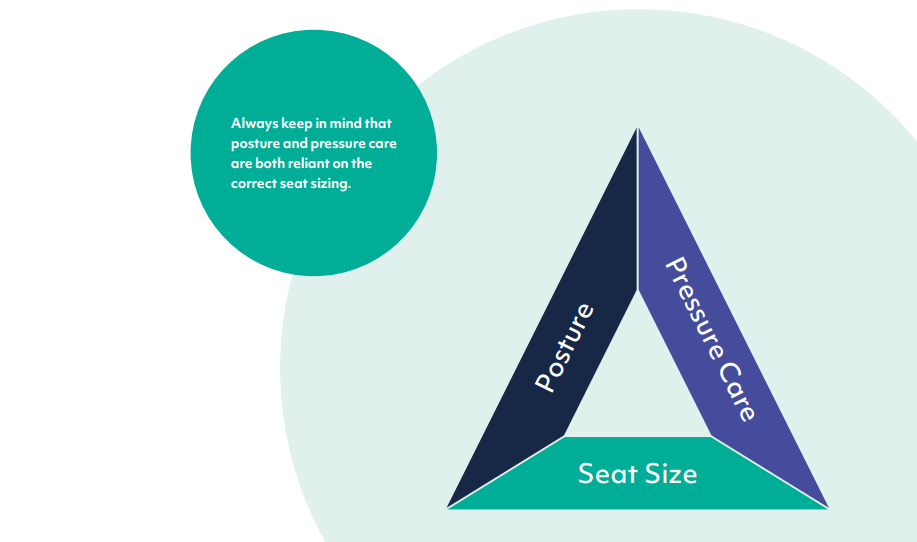
There is a direct relationship between the seat sizing, patient posture and pressure care.
Causes of pressure ulcers in seating
There are many factors that contribute towards the formation of a pressure sores. It may be one of these factors, or it could be a combination of several:
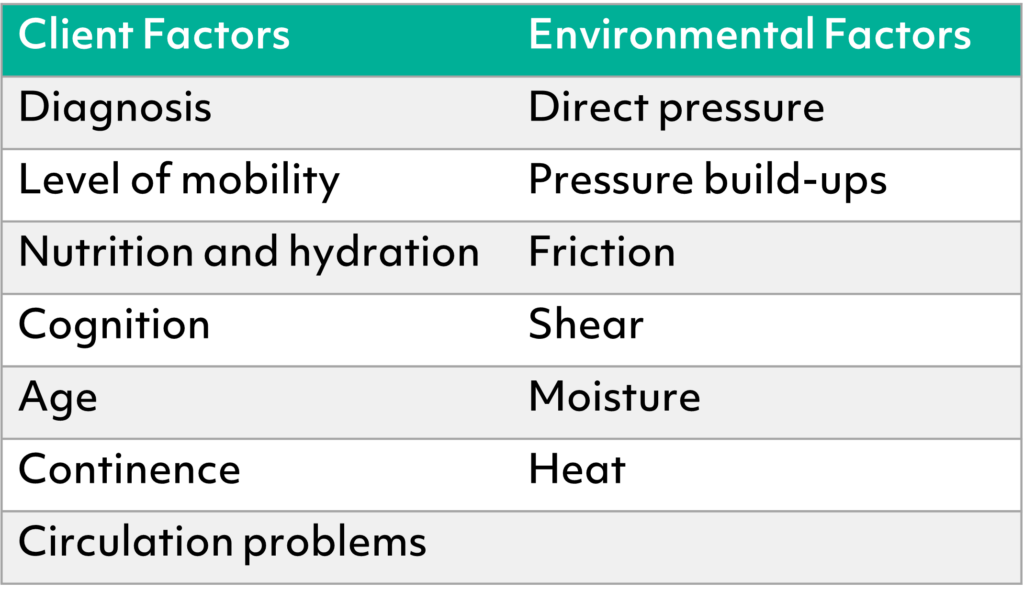
For more information on how pressure effects seating and see a more comprehensive list of causes, download our eBook.
Download our Free Seating Ebook
How to prevent pressure ulcers in seating
By ensuring the client’s body weight is distributed evenly in the chair, we can reduce the degree of pressure on bony areas of the body like the sacrum, elbows, and heels.
Pressure ulcers cause considerable pain, discomfort and cost, and they take much longer to heal than they do to create.
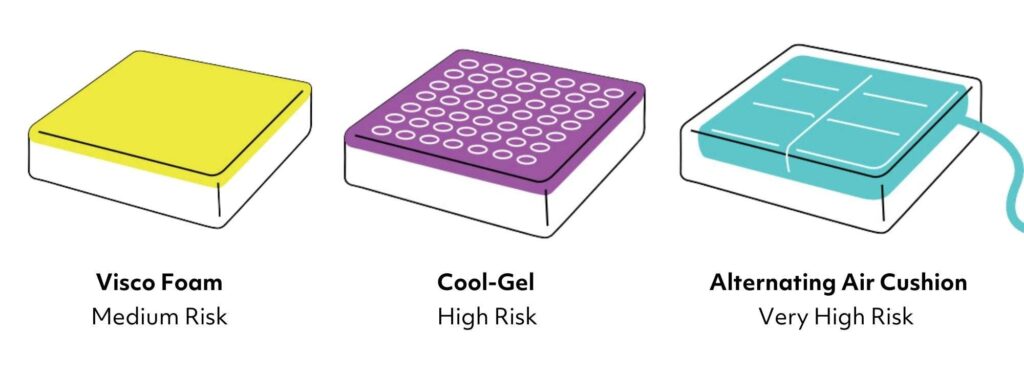
Depending on the age of the client and their skin integrity, different levels of pressure relief will be needed on the contact surfaces of the chair.
So if a patient is at risk, ensure you do something about it. It’s much better to overcompensate and be safe than sorry. Make sure you prescribe something that will suit their future needs as well, particularly if their condition is likely to deteriorate.
Medical conditions and how they impact on seating needs
By having an in-depth understanding of any long-term medical conditions the client has, we can ensure we cater for every aspect of their physical needs.
Stroke Patients
Often a good level of lateral support will be needed for patients rehabilitating from a stroke, as will head support, a tilt-in-space action, and a mobile base. You may want to look for something with flexibility which can be altered to suit the patient’s needs over time.
Spina Bifida
When a baby’s spine and spinal cord don’t develop properly during pregnancy, defects such as a gap in the spine can occur. Physical symptoms of Spina Bifida can include weakness or total paralysis of the legs, incontinence, and a loss of skin sensation in the legs and bottom.
As the condition is from birth, consider a chair that can easily be adjusted in terms of size and support, particularly if they are still growing.
Chairs with fully adjustable backrests are great for Spina Bifida patients, as they can be ‘moulded’ to the shape of the spine to ensure support and comfort and reduce the risk of pressure damage.
Bariatric Clients
Bariatric or plus-sized patients obviously need chairs with a higher weight limit, but your considerations shouldn’t stop there.
Ensure the weight limit includes a safe margin to cope with any fluctuation in body weight over time (you may be wise to check previous medical records to see if this is likely), and to withstand any sudden movements, such as sitting down in the chair suddenly.
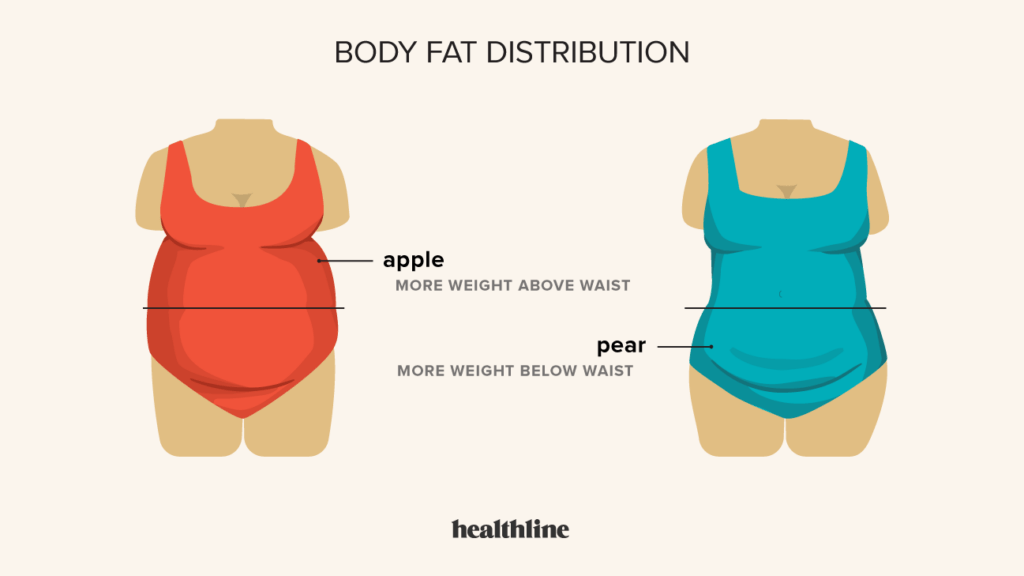
Bariatric Body Shape
Also think about the distribution of weight; clients with oedematous legs may need a reinforced legrest to cope with the extra weight of the swelling. Tilt-in-space with high legrest elevation is a must for clients with oedema.
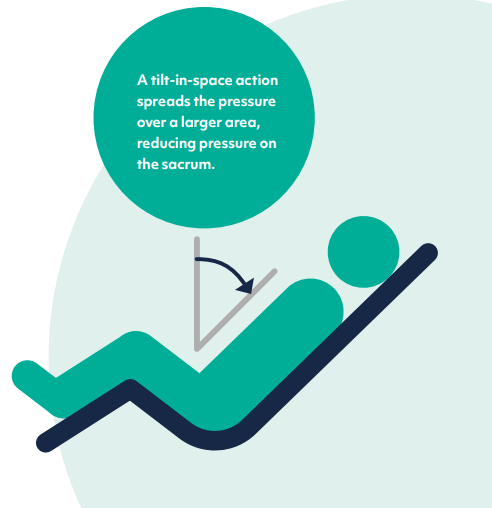
Tilt-in-space functionality
Circulation and Respiratory Needs
Clients with respiratory conditions like COPD, or swelling in their limbs (oedema), need seating that can assist with these problems. A reclining backrest that is angle-adjustable can reduce pressure on the chest to assist with breathing, and an extendable legrest elevates the lower legs to reduce swelling and improve blood circulation.
We’ve covered a range of other conditions in our blog, such as:
- Arthritis, Osteoarthritis, and Rheumatoid Arthritis
- Osteoporosis
- Multiple Sclerosis (MS)
- Dementia / Alzheimer’s Disease
- Brain Injury
- Cerebral Palsy (CP)
- Huntington’s Disease
- Motor Neurone Disease (MND)
- Parkinson’s Disease
- Spinal Cord Injury (SCI)
To find out more about how other medical conditions affect seating, you can download our free eBook.
Download our Free Seating Ebook
Social and Emotional Needs
Having looked at the client’s physical presentation which is predominantly what good seating is about, we should also turn to the client’s emotional needs (we all have them!) and how seating can help improve their wellbeing through greater independence and interaction with their surroundings.
A chair can help improve their social mobility, particularly in communal settings like nursing homes, helping them see their surroundings more easily and maintain eye contact when socialising with other residents. Wheeled castors and push handles can also assist with moving between different rooms throughout the day.
Chair types, categories, and features
When thinking about the type of chair needed, we always ask one question:
Is the patient hoisted?
The client’s level of mobility will determine how much assistance they need with transfers, and the kind of the chair they need, whether this is a riser recliner or care chair.
As a general rule, if the person is hoisted for transfers, a care chair offers better support, is easier to hoist from, and can be wheeled from room to room to cut down on hoisting transfers.

Lento Trio care chair
If the patient is still standing for transfers, you’ll likely be looking at a riser recliner chair or a high back chair.

Riser recliner chair
However, as with any rule, there are exceptions.
Sometimes the client will need the support of a care chair even if they are still standing, and some care chairs will accommodate this.
Other patients may have on and off days — i.e., days when they can stand and days when they need to be hoisted.
In these circumstances, it’s best to make a decision based on:
- Priorities (e.g. is support more important than easy standing transfers?)
- What will be most suitable for them for the majority of days?
- Will their condition change over time – what will be needed in the future?
Key Features to Consider When Specifying New Seating
There are so many features with specialist seating these days that it can be hard to know where to start, but the list below should provide you with a broad overview of some of the most important features to look for.
Adjustability
Adjustability is not only important to adjust the seat size, which can be done easily without tools on our Lento range, but for repositioning the patient and all the health benefits this brings, including extra pressure relief and postural support.
The level of adjustability is different between single and dual motor chairs. Single motor chairs have one rise and one recline action, raising the legs while the tilt-in-space angles the client back in the chair.
Dual motor chairs have a greater level of adjustability, as the backrest and legrest can be adjusted independently for greater postural support.
Ease of Cleaning
The ability to clean the chair easily is important to maintain good infection control, and is especially important if the client has incontinence issues. Chairs good for infection control have waterproof antimicrobial fabrics, removeable cushions, and smooth, recess-free surfaces to prevent the ingress of bacteria.
Stability
Having a robust, well-built frame, and braked castors if the chair is mobile, gives a sturdy chair that keeps the client safe and secure and reduces the risk of falls.
Check the weight limit of the chair as well, standard riser recliners usually have a 25 stone weight limit but bariatric chairs can support up to 50 or 75 stone.
Pressure Care
There are varying levels of pressure relief available in seat cushions, from medium risk foam to coolgel or high-risk alternating air.
Aftersales Backup
Specialist seating is expensive, so ensure the best value for money and longevity of your equipment by checking what level of warranty and aftersales support you have in place.
Options and Accessories
The range of options and accessories available with specialist seating is wide-ranging, such as different backrest styles, inbuilt lateral supports, and add-ons like heat and massage functions and even USB chargers!
Upholstery
The choice of fabric is an important factor in the degree of pressure relief provided. Faux leathers such as Maximo are soft and supple, but also very durable to withstand rigorous cleaning.
Dartex is another clinical-grade fabric that has four-way stretch and antimicrobial properties, providing a cooling effect to keep the skin hydrated, as well as being fully waterproof.
Environmental Considerations
The client’s environment is another aspect to consider in the seating assessment; do they have room to recline the chair, and get out of the chair using standing assistance or hoisting equipment? Ensure that essential items are within easy reach, and the vicinity of the chair is free from clutter to avoid any trips or falls.
Standaid Compatible
The manufacturer’s chair specification should tell you whether the chair is compatible for use with standaids such as the Sara Stedy.
How to measure for seat sizing during a seating assessment
Before we start, here’s a few tips:
- A tape measure with both inches and millimetres is an important part of a seating assessor’s arsenal. Make sure you keep one in your bag!
- Care chairs are often measured in millimetres, with high seats and riser recliners measured in inches. Don’t ask me why, it’s something to do with traditional craftmanship versus modern manufacturing methods for care chairs!
- If you are using a fabric tape measure, don’t let it bend around the body as this can produce a very different measurement.
- It’s best to carry out the assessment in the chair you are prescribing wherever possible. Alternatively, a dining chair works well. In some situations, you may have to measure up whilst the client is in bed, but it’s advisable to work with someone who has done this before if you’re not experienced in this.
- Explain what you will be doing before starting measuring or touching the patient.

A tape measure should be used to take the required measurements
You can read our guide to seat sizing for more in-depth information, but the basic tips for measuring the correct seat dimensions are outlined below:
Back Height
Measure from the top of head to the bottom of the back.
Seat Width
Measure the hip width at the widest point, adding an extra one-inch gap on each side (while ensuring the arms rest comfortably on the armrests).
Seat Depth
Measure from the bottom of the back to the back of the knees, ensuring you can fit a flat hand comfortably between the back of their leg and the legrest.
Floor to Seat Height
Measure from the top of the seat to the floor or footplate, so the client can comfortably support themselves with their feet resting flat.
Arm Height
Measure from the top of the seat to the top of the armrest, the client’s shoulders should be relaxed with their arms resting comfortably on the armrests.
Justifying your seating prescription decisions
If you are a healthcare professional, there are a few reasons why you should document your findings and justify the seating decisions you have made:
- Legal reasons — As part of your duty of care towards your client, you need to record why the seating was chosen.
- To aid future care – You may want to refer to your prescription in the future to see how their needs have change.
- To obtain funding – If you are applying for funding, most funding providers will need to see a seating justification
- To outline your reasoning – It can be helpful for all parties involved to revisit why seating features were specified in the first place.
After the seating assessment
Seating provision doesn’t just stop at the assessment, there are still some important steps to take:
- Chair setup — Make sure the chair is adjusted correctly for the patient, otherwise it won’t do its job properly!
- If relevant, create a seating care plan to document how the chair should be setup, how the client should be seated, and how long for.
- Train the patient, carers, or family members on the correct use of the chair.
- Schedule return visits to reassess the client and adjust the chair if necessary.
A final word
With decades of experience carrying out seating assessments, we are well-placed to advise therapists, carers and the clients themselves about the best ways to conduct a seating assessment to get the best clinical outcomes.
If you want take a deeper dive into this subject, download our “Healthcare Professional’s Complete Guide to Specialist Seating Assessments”.
Or book a no-obligation seating assessment with one of our seating experts!
Free & No Obligation Assessment
Frequently Asked Questions
What is a specialist seating assessment?
A specialist seating assessment is a detailed evaluation of an individual’s seating needs to ensure comfort, safety, and postural support. It considers factors such as mobility, posture, pressure care, and medical conditions to recommend the most suitable seating solution.
What is included in a seating assessment checklist?
A seating assessment checklist typically includes:
Medical history and mobility status
Postural seating evaluation
Risk of pressure ulcers
Functional needs and daily activities
Seat sizing (height, depth, width, armrests)
Transfer methods (standing, hoisting, or assisted transfers)
Environmental considerations (home, care facility, or workplace)
How does a chair assessment help with patient comfort?
A chair assessment ensures that the chosen seating solution meets the patient’s physical and medical needs. It helps prevent discomfort, pressure sores, and poor posture by selecting the right chair type, size, and features.
What is postural seating, and why is it important?
Postural seating refers to seating solutions designed to support proper spinal and pelvic alignment, reducing pain and preventing deformities. It is crucial for individuals with limited mobility, neurological conditions, or musculoskeletal disorders.
What is a care chair, and who needs one?
A care chair is a specialist seating solution designed for individuals who require high levels of support and assistance with transfers. These chairs often include tilt-in-space functions, pressure relief features, and adaptable positioning to enhance comfort and safety.
How can I get a specialist seating assessment?
A specialist seating assessment is typically conducted by an occupational therapist, physiotherapist, or seating specialist. Contact your local healthcare provider or a specialist seating company to arrange an assessment.














