The importance of early mobilisation in a hospital patient’s recovery programme cannot be underestimated.
Prolonged bedrest can produce a variety of complications, as explained in this article, that cause patients’ health to deteriorate, extending their hospital stay.
On the contrary, mobilising the patient early from their bed to their chair and beyond, helps them rehabilitate quicker and strengthens them for discharge. This reduces the number of patient bed days for the hospital, reducing cost, and reduces the likelihood of the patient being readmitted to hospital, as they are stronger and able to live more independently.
Jump straight to...
The Problem
Delays in mobilisation of hospital patients and the resulting decrease in their mobility following treatment or surgery, inevitably results in poorer health outcomes for them.
Unfortunately, there are many factors that encourage this poor practise of leaving patients in bed and not mobilising them soon enough.
- Pain – joint pain/arthritis can mean patients cannot reposition themselves and are unable to get mobile.
- Fear of falling — learned fear of falling and injuring themselves means patients are reluctant to stand on their feet and walk between their bed and chair.
- Unsuitable bed/chair. The bed or chair is not fit for purpose, preventing them from getting up because of the wrong height chair, or the bed does not profile or adjust to the right height.
It is important for the moving & handling practitioners to be involved as much as possible in helping the patient mobilise.
The Effects of Delayed Mobilisation
- Decreased muscle mass and bone density. Muscle loss in the elderly (sarcopenia) is driven by a reduction in muscle protein synthesis, due to lack of movement. Studies have shown that older adults can lose up to 1kg of muscle mass in 10 days of bedrest.
- Skin deterioration. Prolonged bedrest poses a risk to skin integrity, if there is constant pressure on certain areas of the skin. This compresses the skin tissue, causing a loss of blood flow and skin tissue to break down.
- These factors compromise the patient’s health and make it harder for them to regain full strength. The seriousness of deconditioning cannot be underestimated. It takes twice as long to recover mobility as it does to lose it!

Delayed bedrest is often referred to within the NHS as ‘pyjama paralysis’. For many patients, being in their bedclothes all the time reinforces the feeling of being ill, preventing a speedy recovery. Studies have shown that 3 out of 5 elderly patients that were immobilised in bed had no medical reason for needing bedrest.
At the end of last year, 13,440 patients per day were remaining in hospital that were medically fit to be discharged, 30% more than the previous year. Patients with prolonged hospital bedrest are at greater risk of picking up HAIs (Hospital Acquired Infections) and increased frailty, weakening their health further and extending their hospital stay.
Steps to Resolving the Problem
Upgrading equipment is a key part of the solution, as a lot of existing beds and chairs on hospital wards are antiquated and there is a severe lack of bedside chairs compared to beds.
Without having the right equipment to mobilise patients, staff become the equipment! They become heavily involved in moving the patient manually in the bed or chair, taking up extra carer resource and increasing staff musculoskeletal disorders (MSDs) due to constant strain. With the right equipment in place, staff can spend less time manual handling, and more time moving & handling the patient with the right equipment!
The NICE guidelines around moving patients regularly need to be recognised. As already mentioned, it imposes significant strain on the staff if the right equipment is not available, strengthening the need to have the suitable chairs and equipment in place to assist staff with the moving & handling process.

The Importance of Having the Right Chair
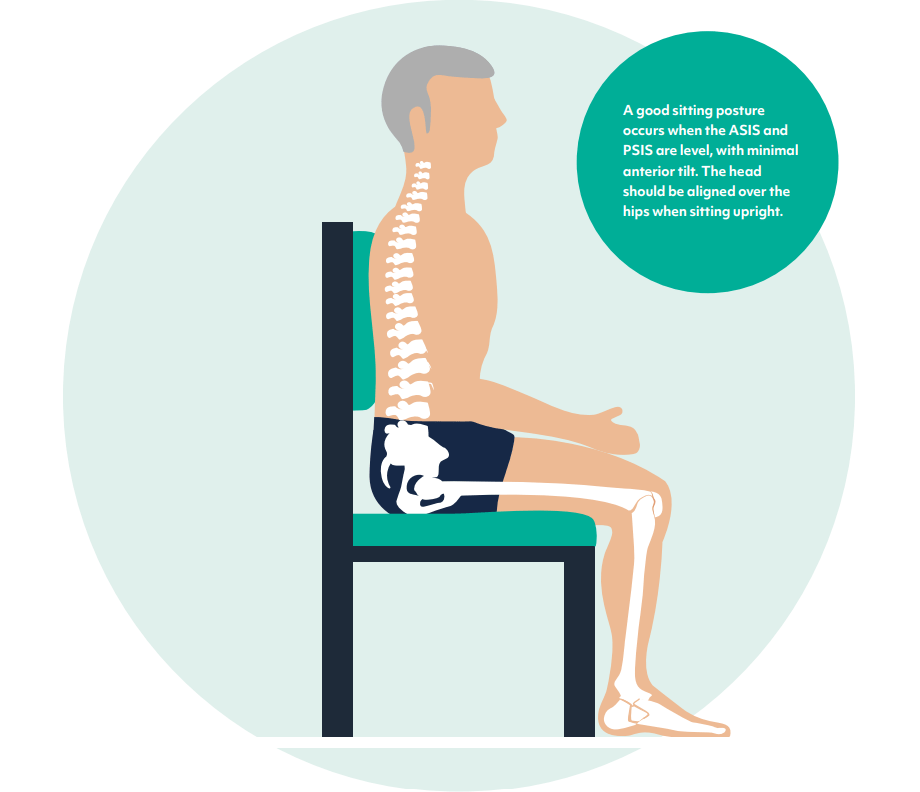
The following points show how fundamental it is to have the right kind of chair for the patient.
- It ensures they maintain the right posture in the chair, preventing any musculoskeletal problems from developing.
- It aligns their posture correctly, so they are seated centrally in the chair and not leaning to one side, which significantly reduces the chance of pressure sores.
- The patient should be able to stand up easily from the chair, by moving forward in the chair and pushing down on the armrests.
How to Check if the Patient has Suitable Seating
Each patient admitted onto the ward should have a baseline seating assessment, which can be carried out by any manual handling care staff. A baseline seating assessment is to be distinguished from a therapist’s seating assessment. A therapist’s assessment will be more detailed and look at the whole picture of client needs, and while this is very much needed, staff shouldn’t wait for a therapist to get involved, but ensure the seating passes some basic tests as soon as the patient arrives on the ward.
The baseline assessment will check that the chair meets the following requirements:
- Correct hip to knee angle for the patient
- Correct armrest height
- Patient’s feet are flat on the floor or footrest
This should be documented as part of the initial Patient Mobility Assessment.

Other seating features can help further with rehabilitation, such as tilt-in-space, articulating legrests and graded vertical rise.
- Tilt-in-space. This rocks the angle of the patient back in the chair, whilst keeping the same sitting profile, which redistributes the weight of the patient across their body and relieves pressure.
- Articulating legrests. These extendable legrests pull forward to provide contact support all the way up to the calf and knee, preventing the build up of fluid (oedema).
- Graded vertical rise. This rise function in the chair rises vertically at first, then angles forward slightly, to stabilise the patient and help them get to their feet more gradually if they are weaker physically.
Staff Involvement
It is critical to train staff so they know how to operate the equipment correctly. Something as simple as adjusting the chair height might be avoided if the staff are unsure, or it is too difficult or time-consuming to carry out. Simple mechanisms that can be adjusted with minimal hassle are the way forward, and reduce staff time spent on manual handling.
Overcoming Resistance to Change
Cultural norms and retaining the status quo can be a strong barrier to more effective clinical practices. It can be beneficial for those proposing change in the organisation to make a ‘business case’ for the overall effect the change will have on patient and care organisation, including money and time saved.
We have lots of free resources and justification templates to help you put a together a strong business case, where there is a need for better equipment. Check out the resources section on our website for these free downloads!
Sometimes it can even be the patient themselves that is resistant to change, even when there is a clear need for better equipment to help them recover. This can be due to fear, misunderstanding or lack of cooperation due to their overall wellbeing and state of mind. Listening to the patient, agreeing with them and making them feel they are deciding for themselves in their own best interests can all help to get them on board.

The Solution
The end goal in mind, which is always to be kept front and centre when reviewing mobility equipment in hospital wards, is helping to mobilise the patient from their bed into a suitable chair, which will ultimately aid recovery and make them fit for discharge back into the community.
The correct seating for early mobilisation should include the following features:
- Easy height adjustment. Awkward leg adjustment mechanisms will put staff off because of the time and strain involved, but height adjustment is essential to make the chair suitable for each different patient.
- The appropriate level of support. The chair should be comfortable with sufficient padding and support on the seat, armrests, and have the right back profile to support their head and neck, without creating any pressure points which could lead to skin integrity issues.
- Good neck position. The back of the chair should be straight with the correct support around the neck e.g. a neckroll on weighted flap.
- Sling compatibility. As well as being compatible with a standaid, the chair needs a gap between the seat and backrest to facilitate attaching a sling to the patient, to help them stand up in the early stages of recovery.
A natural by-product of suitable ward seating will be reduced staff workload, as patients mobilise quicker and increase their independence.
Speak to Our Acute Seating Team for More Advice on Ward Seating