Pressure sores will affect 700,000 people in the UK this year. 100,000 of those pressure injury incidents will be newly acquired.
The importance of correct pressure care management cannot be overlooked. In 2015-16, treating pressure damage costs the NHS more than £3.8 million every day.
For this reason, NHS England have described managing injuries & preventing the development or pressure sores as a “priority for policy makers, managers & practitioners alike”.
With this in mind, let’s look at the definitions, symptoms, grading and potential treatments of pressure sores.
Jump straight to…
What Are Pressure Sores?
Pressure ulcers, or pressure sores are injuries to parts of the skin that have been placed under pressure for a long period of time because a person is unable to move or change position.
They usually develop over time but can sometimes form in just a couple of hours.
Why Do They Develop?
Pressure sores develop when pressure is applied to part of the skin for a long time and cuts off the blood supply. They can lead to break downs in the skin and, in serious instances, the tissue beneath the skin.
In the most severe cases, pressure ulcers can lead to the skin on the affected area eventually dying.
Moisture on the skin can also increase the chances of a pressure sore developing. They are a constant issue for patients in low mobility scenarios.
From acute care settings to community and residential care, any situation where patients can be sat or laid on inadequate surfaces for prolonged periods of time is one where pressure ulcers are likely to develop.
Sitting, sleeping or lying on the correct type of surface decreases the chances of developing pressure injuries & can even manage existing pressure sores as well as prevent them from becoming more severe.
What Are the Symptoms of Pressure Sores?
Symptoms of pressure ulcers can include swelling and changes in skin colour, warmth, tenderness, and pain in the affected area.
A pressure sore has begun to form if pressure is removed from the affected area and the skin doesn’t return to normal after 10-30 minutes.
People with white skin tend to get red patches, while these same pressure ulcers tend to be purple or blue on people with dark skin.
If untreated, skin may crack and leave an individual very susceptible to infection.
Who is at Risk of Pressure Sores?
Pressure injuries can happen to anyone that is sat or laid down for a prolonged period of time. There are more common in people with low mobility who spend lots of time in a chair or bed.
Older adults are the most likely to develop a pressure ulcer, one reason for this is that hospital admission generally increases the chances of developing a pressure sore.
The incidence of pressure ulcers in hospitals amongst inpatients is 3-14%, this can be as high as 70% in patients with orthopaedic problems.
It is incredibly important that proper pressure care is practiced, not only to avoid worsening of a pressure injury, but to reduce the likelihood of a patient being hospitalised.
Pressure ulceration in elderly patients is associated with a fivefold increase in mortality.
This means that, particularly for the elderly, any illness that may increase the chances of being hospitalised also increases the likelihood of developing a pressure ulcer because of hospitalisation.
How Common are Pressure Sores?
In the UK, just under half a million people will develop at least one pressure ulcer in any given year.
Pressure injuries are most common in people with underlying health conditions as this is who is most likely to spend long periods of time in a hospital bed or wheelchair.
Around 1 in 20 people that are admitted to a hospital with a sudden illness will develop a pressure ulcer.
People over 70 are the most vulnerable as they are likely to have low mobility and ageing skin, this group is also very likely to be hospitalised.
Between 2015 — 16, the cost of treating pressure injuries and the damage they cause was more than £3.8 million every day
Can Pressure Sores get Worse?
Yes, pressure injuries can worsen and even become life threatening if not properly treated. Due to the ease in which these sores can be infected, it is of paramount importance that proper wound treatment is practiced.
Proper nutrition, consistent wound treatment and regularly offloading pressure from the affected area can help prevent the worst outcomes.
What is a Sacral Pressure Sore?
Sacral pressure sores are a very common type of injury, this refers to a pressure sore that occurs in the sacrum which lies between the fifth segment of the lumbar spine and the coccyx.
Sacral pressure is what most people have experienced when sitting on a hard surface for a long period.
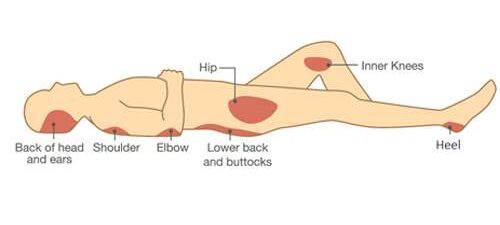
Sacral pressure sores are common as pressure sores tend to form on the skin covering bony areas of the body such as:
- Buttocks
- Back
- Tailbone
- Hips
- Elbows
- Heels
- Ankles
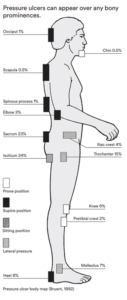
Skin that is over bony prominences is most at risk of developing pressure sores. These areas require the most protection offered from the correct equipment.
Pressure or Bed Sore Grading
When pressure ulcers occur and damage the skin, they can do so at varying levels depending on how long an individual has been confined the position that caused the ulcers.
The severity of pressure ulcers is measured on a grading scale (Grade 1 — 4), there are 6 categories of bed sore grading with grade 4 pressure sores being the most serious.
Bed sore grading ranges from grade 1-4 and each one becomes progressively more serious.
Grade 1 Pressure Sore
- Grade 1— Skin discolouration, usually red on light-toned skin or purple/black if more severe
- Blueish/purple on darker toned skin.
Grade 2 Pressure Sore
- Grade 2 — some skin damage or loss involving the top skin layers
Grade 3 Pressure Sore
- Grade 3 — necrosis (death) or damage to the skin patch, limited to the skin layers
- Deep wound that may extend further than the original wound
Grade 4 Pressure Sore
- Grade 4 — necrosis (death) or damage to the skin patch and underlying tendons, joint or bone
- Exposes muscles, bones, and tendons to infection
Grade 3 and Grade 4 bedsores are almost like an open door for bacteria and infection. It is very important that this level of injury is treated immediately by a medical professional.
Deep Tissue Injury
A Deep Tissue Injury (DTI) is a type of tissue damage that is slightly different to a pressure ulcer.
Pressure ulcers usually come with a breakage of the skin, but a deep tissue injury is not always associated with broken skin and does not always become the open wound but is still defined as a pressure ulcer.
The European Pressure Ulcer Advisory Panel (NPUAP) updated their definition of pressure injuries in 2007 to include DTIs.
Pressure related Deep Tissue Injuries commonly occur at the areas that are most susceptible to pressure injuries like the heels, sacrum, and buttocks.
Unstageable Pressure Sore
- Ulcer that has full thickness tissue loss but is either covered by extensive dead necrotic (dead) tissue or by an eschar.
- The base of the ulcer is covered by slough (yellow, tan, grey, green or brown)
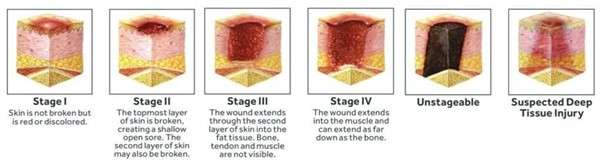
Pressure ulcer stages
Mucosal Membrane Pressure Injury
This is a type of pressure injury that occurs when pressure is applied to a ‘mucous membrane’.
This is a moist lining in tracts & passages in the body like the nasal passages, gastrointestinal & urinary tracts. When pressure is applied to this tissue, it can lead to ulcers developing. These tissues are vulnerable to pressure from medical devices like oxygen tubes and catheters.
Because of this, Mucosal Pressure Ulcers (MPrU) are pressure ulcers found on mucous membranes with a history of a medical device in use at the location of the ulcer.
Can Pressure Sores be Treated?
Yes, pressure sore treatment is possible, but is also dependent on the severity. Many experts strongly believe that bedsores shouldn’t ever get past the first stage.
Low grade (stage 1 & 2) pressure sores can be an inconvenience that usually requires basic nursing care.
Medium to high grade (stage 3 & 4) pressure sores can be extremely serious; they can leave a person susceptible to infections and cause life-threatening complications like blood poisoning.
Treating unstageable pressure sores is a longer process, the pressure wound is first put through a debridement process where the wound is cleaned, infected tissue and other debris is removed.
Debridement is done so that the wound can be properly staged and treated.
How to Treat Pressure Sores
There are various treatment methods available for multiple stages of pressure injuries and the correct treatment method varies depending on the seriousness of the ulcer.
- Relieve pressure through regular movement and position changes
- Apply dressings that speed up the healing process
- They may also help to relieve pressure
- Bandaging with gauze, foam, or other options
- Using specially designed static foam mattresses or cushions
- Or dynamic mattresses and cushions that pump a constant flow of air
- A procedure to clean the wound and remove the damaged tissue (debridement)
Dressings for Pressure Sores
Various dressings are available as treatment for pressure sores, they can be used to protect pressure injuries and speed up the healing process.
Alginate dressings — this type of pressure sore dressing is made from seaweed and contains sodium & calcium which are both known to speed up the healing process
Hydrocolloid dressings — this type of pressure ulcer dressing contains a gel that encourages growth of new skin cells in the ulcer and keeps the surrounding skin healthy
Other dressings for pressure sores — these can be foams, film, hydrofibres/gelling fibres, gels, and antimicrobial (antibiotic) dressings can also be used
Pressure Sore Cushions & Mattresses
There are additions to chairs and beds that can be made to relieve or prevent pressure ulcers.
A pressure sore cushion for chair can come in a simple square or rectangular shape, or as a wedge to place on your regular seating area.
A pressure sore mattress acts in the same way but for the entire body, they are filled with foam that relieves pressure put on areas of the skin can prevent pressure injuries.

Airflow mattress
Take a look at our beds & mattresses range for pressure care management. With options to care for low grade pressure injuries as well as high grade pressure sores that require more specialist attention.
Moisture Barrier Cream
This is a cream that protects the skin’s exposure to moisture, urine & stool. Moisture increases the likelihood of a pressure ulcer forming and a barrier cream reduces the risk of this happening.
Antibiotics
For the highest grades of pressure sores, antibiotics may be prescribed to treat an infected ulcer. These infections can be:
- Blood poisoning — also known as sepsis
- Bacterial infection — known as cellulitis
- Infected bone — osteomyelitis
Diet & Nutrition
Diet & nutrition will not stop pressure injuries from developing if you are resting on imperfect surfaces, but a diet containing a good amount of protein and a variety of vitamins & minerals can also speed up the healing process. It is also important to stay well hydrated as dehydration can slow down the healing process.
Summary
The legendary public health figure Florence Nightingale once said, “If he [the patient] has a bedsore, its generally not the fault of the disease but of nursing”.
This view is also echoed by today’s pressure care experts who believe that pressure sores can be avoided with proper procedure and recommend that skin assessments for patients at risk of pressure ulcers should be completed at least once a day.
The problem of pressure injuries has increased in modern times as people live for longer and obesity increases, but pressure sores are highly preventable, therefore healthcare professionals must use the correct equipment and strive to give patients proper care.
Take a look at our specialist seating & range of care beds & mattresses to see how our products could offer you the pressure injury management that you need.
Alternatively contact us and talk to one of our expert seating specialists who will guide you through our price range, ensuring we find the right seating for managing pressure injuries.
Get Expert Advice
FAQs
What are the typical symptoms of pressure sores?
Common signs include skin discoloration, swelling, tenderness, and pain. Advanced sores may lead to cracked skin and infection.
Bed Sore Grading: How are bed sores graded?
bed sores are categorised into four grades based on severity, ranging from discoloured skin (Grade 1) to exposed bone (Grade 4).
Grade 1— Skin discolouration, usually red on light-toned skin or purple/black if more severe
Grade 2 — some skin damage or loss involving the top skin layers
Grade 3 — necrosis or damage to the skin patch, limited to the skin layers
Grade 4 — necrosis or damage to the skin patch and underlying tendons, joint or bone
Can pressure sores be treated?
Yes, treatment options include repositioning, specialised cushions and seating, wound care, and in severe cases, debridement and antibiotics.
How long do pressure sores take to heal?
The healing time for pressure sores (also called bedsores or pressure ulcers) depends on several factors, including the severity of the sore (categorized into stages), the individual’s overall health, and the quality of care received.
Here’s a breakdown of healing time based on the stages of pressure sores:
Stage 1: A few days to 1 week with proper care, including relieving pressure on the affected area.
Stage 2: 1 to 3 weeks with treatment such as cleaning the wound, keeping it moist, and relieving pressure.
Stage 3: 1 to 4 months depending on the extent of tissue damage and the care provided. Healing is slower than in earlier stages.
Stage 4: 3 months to 2 years or even longer. Healing can be very slow, and often requires specialized wound care and sometimes surgery.
Severe pressure sores (Stage 3 or 4) may never fully heal in some cases, especially in individuals with limited mobility or other complicating health conditions. Early intervention and prevention are critical.