Preventing pressure ulcers (also known as pressure injuries or bedsores) is crucial when caring for individuals with limited mobility. These painful conditions occur due to prolonged pressure on the skin, leading to tissue damage. However, by implementing appropriate preventive measures like regular repositioning techniques and specialised pressure ulcer prevention equipment, caregivers can significantly reduce the risk.
This article provides an in-depth guide on understanding pressure ulcers, the importance of repositioning, various equipment options available, and best practices for nursing care.
Jump straight to…
Understanding Pressure Ulcers
Pressure ulcers develop when continuous pressure restricts blood flow to a specific area, causing tissue damage. They commonly occur in bony parts of the body, such as the sacrum, coccyx, hips, heels, and shoulder blades, which bear the most weight. Key factors contributing to pressure ulcer development include immobility, friction, moisture, poor nutrition, and medical conditions affecting circulation.
Repositioning as a Preventative Measure
Regular repositioning is a fundamental strategy to prevent pressure ulcers in patients with limited mobility. By redistributing pressure, repositioning helps alleviate stress on vulnerable areas and promotes healthy blood flow. It is recommended to reposition patients at least every two hours, but individual needs may require more frequent adjustments.
Caregivers should use proper lifting techniques to prevent injury and consider supportive aids like slide sheets or transfer boards to minimise friction and shear forces during repositioning.
Specialist Care Equipment for Pressure Ulcer Prevention
In addition to repositioning, various equipment options can assist in preventing pressure ulcers in low mobility patients. Let’s explore some of these tools and their benefits:
1. Riser Recliner Chairs:
Riser recliner chairs play a crucial role in pressure ulcer prevention for low mobility patients. These chairs provide adjustable seating positions, allowing patients to relieve pressure on specific areas of their bodies.
By promoting proper posture and weight distribution, riser recliner chairs help reduce the risk of pressure ulcers, providing comfort and support.

The Lento Mobile Riser Recliner chair offers a range of features ideal for the care of low mobility patients, ensuring comfort and support.
2. Profiling Beds:
Profiling beds are essential for patients at risk of pressure ulcers. These beds feature multiple adjustable sections, enabling caregivers to customize the bed’s position to meet the patient’s needs. By adjusting specific areas such as the head, feet, or mid-section, profiling beds help distribute pressure evenly, minimizing the risk of pressure ulcers and ensuring proper body alignment.

An electric profiling care bed is perfect for elderly individuals, offering adjustable sections to optimize comfort and pressure relief.
3. Tilt-in-Space Chairs:
Care chairs designed for pressure ulcer prevention are equipped with features that prioritise patient comfort and reduce the risk of pressure ulcers. These chairs often come with specialised cushions that offer pressure redistribution and support.
The cushions can be made of foam, gel, or use alternating air technology. Foam cushions provide stability and contouring, gel cushions offer enhanced immersion and pressure relief, while alternating air cushions dynamically redistribute pressure, reducing the risk of pressure ulcers. Additionally, these wheelchairs have adjustable seat angles to optimise seating positions and minimise pressure on vulnerable areas.
Tilt-in-space chairs allow the entire chair to tilt, redistributing pressure and providing optimal seating positions for individuals with limited mobility. This feature not only enhances comfort but also helps in pressure redistribution, making these changes highly effective in pressure ulcer prevention.

The Lento Patient Care Chair can tilt and provide an elevated footrest, offering improved support for patients with complex conditions.
4. Tilt In Space Wheelchairs:
Tilt-in-space wheelchairs designed for pressure ulcer prevention are equipped with features that prioritise patient comfort and reduce the risk of pressure ulcers. These wheelchairs often come with specialised cushions that offer pressure redistribution and support.
Foam cushions provide stability, gel cushions offer enhanced immersion and cooling, while alternating air cushions dynamically redistribute pressure, reducing the risk of pressure ulcers.
Tilt-in-space wheelchairs feature specialised cushions, adjustable seat angles, and pressure redistribution mechanisms. These features optimise seating positions, minimise pressure on vulnerable areas, and enhance patient comfort.

Tilt-in-space wheelchairs tilts to evenly distribute pressure across the users body.
5. Pressure Cushions:
Pressure relief cushions like foam, gel, and alternating air cushions are widely used to prevent pressure injuries. These cushions aid in pressure redistribution and provide comfort. They are ideal for patients at high risk of developing pressure injuries.
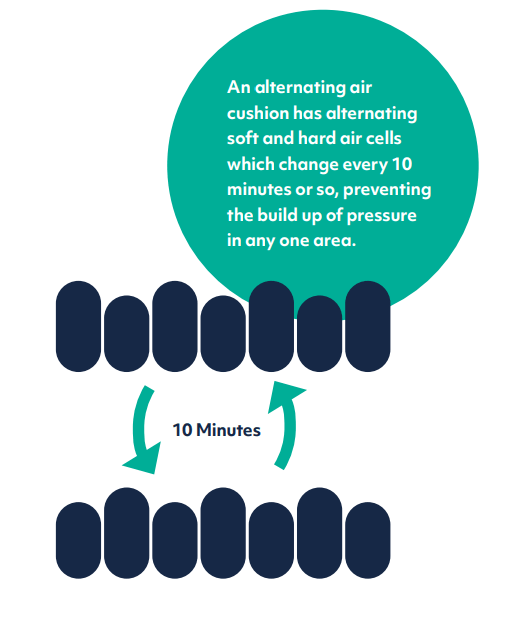
Alternating Air Cushions are recommended for patients at the highest risk, as they dynamically adjust to redistribute pressure and prevent skin breakdown.
Best Practices for Pressure Ulcer Prevention in Nursing Care
To effectively prevent pressure ulcers in low mobility patients, it’s crucial to adopt a comprehensive approach. Here are some best practices for pressure ulcer prevention:
• Perform regular skin assessments: Conduct thorough skin checks at least once a day, focusing on high-risk areas. Document any changes, such as redness, swelling, or breaks in the skin, and notify the healthcare team immediately.
• Maintain skin hygiene: Keep the skin clean and dry to minimize infection risk. Use gentle cleansers and moisturisers recommended by healthcare professionals, avoiding harsh soaps or excessive rubbing.
• Optimize nutrition and hydration: A balanced diet rich in protein, vitamins, and minerals is essential for maintaining healthy skin. Adequate hydration also plays a key role in skin health. Consult a registered dietitian for personalised dietary plans.
• Educate patients and caregivers: Empower patients and their caregivers with knowledge about pressure ulcer prevention, including the importance of repositioning, skin care, proper nutrition, and the correct use of equipment. Encourage regular follow-ups with healthcare providers.
Conclusion
Preventing pressure ulcers in low mobility patients requires a multifaceted approach, including regular repositioning, the use of specialised equipment like riser recliner chairs, profiling beds, and tilt-in-space wheelchairs. Comprehensive nursing care, including daily skin assessments, maintaining hygiene, optimising nutrition, and educating patients and caregivers, is vital for effective prevention.
By integrating these strategies into daily caregiving routines, healthcare providers can minimize the occurrence of pressure ulcers, enhance patient comfort, and improve the quality of life for individuals with limited mobility.
Remember: each patient is unique, and care plans should be tailored to individual needs in consultation with healthcare professionals.
Get Expert Advice
Frequently Asked Questions (FAQ)
What are pressure ulcers, and why are they a concern for low mobility patients?
Pressure ulcers, also known as bedsores or pressure injuries, occur when prolonged pressure restricts blood flow to the skin, causing tissue damage. They are a significant concern for low mobility patients who are unable to change positions frequently, increasing their risk of skin breakdown.
How often should patients be repositioned to prevent pressure ulcers?
To prevent pressure ulcers, it’s generally recommended to reposition patients every two hours. This helps to redistribute pressure and improve blood flow, reducing the risk of pressure injuries. However, some patients may need more frequent repositioning based on their condition.
How do riser recliner chairs help with pressure ulcer prevention?
Riser recliner chairs are designed to adjust seating positions, offering pressure relief to specific body areas. By promoting better weight distribution and posture, they help prevent pressure injuries in patients with limited mobility, making them a valuable tool in pressure ulcer prevention.
What is the benefit of using a tilt-in-space wheelchair for pressure ulcer prevention?
A tilt-in-space wheelchair allows the entire seating area to tilt, shifting pressure away from high-risk areas. This pressure redistribution minimizes the risk of pressure injuries, making it ideal for low mobility patients who spend long periods seated.
Which type of pressure cushion is best for preventing pressure ulcers?
The choice of pressure relief cushion depends on the patient’s needs:
Foam cushions offer stability and basic support.
Gel cushions provide cooling and enhanced immersion.
Alternating air cushions dynamically shift pressure points, ideal for high-risk patients.
Consult a healthcare provider to choose the best cushion based on individual risk factors.