The EPUAP (European Pressure Ulcer Advisory Panel) defines a pressure ulcer as a “localised injury to the skin and/or underlying tissue usually over a bony prominence, as a result of pressure, or pressure in combination with shear”. Alternative terms include pressure sores, pressure wounds or decubitus ulcers.
Pressure wounds are widespread issue in healthcare environments, 4 million people throughout Europe are affected by them and they cost an astonishing £60m per year to treat.
There are many organisations dedicated to combating this global issue. The EPUAP is a European-wide research group that aims to influence public policy and educate, publishing guidelines in each member country for health and social care bodies to follow.
The NPIAP (National Pressure Injury Advisory Panel) is a not-for-profit organisation composed of healthcare professionals, dedicated to the prevention and management of pressure injuries.
EWMA (European Wound Management Association) is an umbrella organisation, working in association with different pressure ulcer groups to achieve its goals of advancing education and research about this issue.
TVS (Society of Tissue Viability) is a member-led organisation, and brings together clinical experience to create solutions to tissue viability challenges, and implement these within healthcare environments.
Jump straight to...
Who is Most Susceptible to Pressure Ulcers?
Everyone who is immobilised for a prolonged period of time, most likely due to hospital treatment, is susceptible in some way to a pressure ulcer starting to form, without carrying out any prevention techniques.
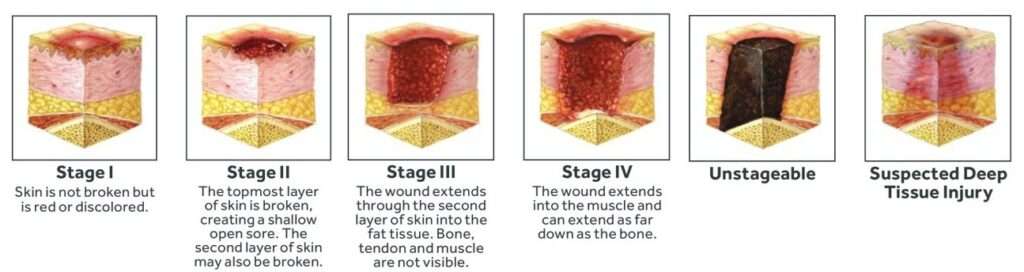
Stages of pressure ulcer development
Some groups of people are more susceptible due to the nature of their existing conditions, these include the following patient demographics:
Diabetics
These patients are more susceptible because of nerve damage and poor circulation. Nerve damage means they may lose sensation in certain areas such as the feet which means they are not aware of pressure or friction in this area. Poor circulation means weaker blood flow, so blood may not circulate as well to extremities like the feet and hands, causing skin tissue to degenerate more easily.
Spinal cord Injuries
Patients with spinal cord injuries are more at risk of pressure injuries due to nerve damage making them more immobile, and possibly unable to change their position due to paralysis.
Reduced Mobility
Patients with joint/muscle weakness and poor mobility generally will have difficulty moving and changing their position, and will tend to be confined to bed for longer periods if they are unable to walk or move themselves independently.
Sensitive skin
Weaker skin that is more fragile will break down more easily from pressure and shear friction.
EPUAP 2023
The European Pressure Ulcer Panel met in Leeds, UK in 2023 for their annual conference and exhibitor event. The main theme of this event was innovation in pressure ulcer prevention and treatment. Our seating solutions and rehabilitation products focus on innovative prevention technologies in pressure care. We showcased these solutions at Stand 18 during the 3-day show which ran from 13-15 September.

EPUAP 2023 venue: The Royal Armouries Conference & Events Centre
The main topics covered during the event were:
Person-Centred Treatment
Person-centred treatment is increasing in focus and helps create a more joined-up care plan around the multiple needs of one individual patient, avoiding crossover, duplication and gaps in care provision.
Risk Assessments
The role of risk assessments has never been greater in pressure care prevention, helping care staff take account of a range of holistic factors, such as pre-existing conditions, and factor these into the care plan to minimise risk. The more work that goes into prevention of pressure ulcers, the lower the treatment cost and length, and better the treatment outcomes for the patient.
New Technologies and Innovations
Extensive research is going into improving treatment of pressure ulcers. The symposia workshops throughout the EPUAP event will be demonstrating many of the latest innovations in pressure ulcer management. There is a current emphasis on involving service users in the research and development stage, to utilise their first-hand experience in being treated for pressure ulcers.
The Role of Seating in Pressure Care
Patient seating can go a long way in reducing the chances of pressure ulcers with the right fabrics and features. These are some of the essential features for good pressure relief.
Pressure-Relieving Material
A soft breathable fabric on the contact areas, such as polyurethane or vapour-permeable material like dartex, prevents the build up of pressure and moisture, keeping the patient’s skin well-ventilated and comfortable. The 4-way stretch properties in the fabric allow for greater pressure distribution and reduce friction on the skin. We incorporate these fabrics in our seating range to assist pressure care and help infection control with easy cleaning.
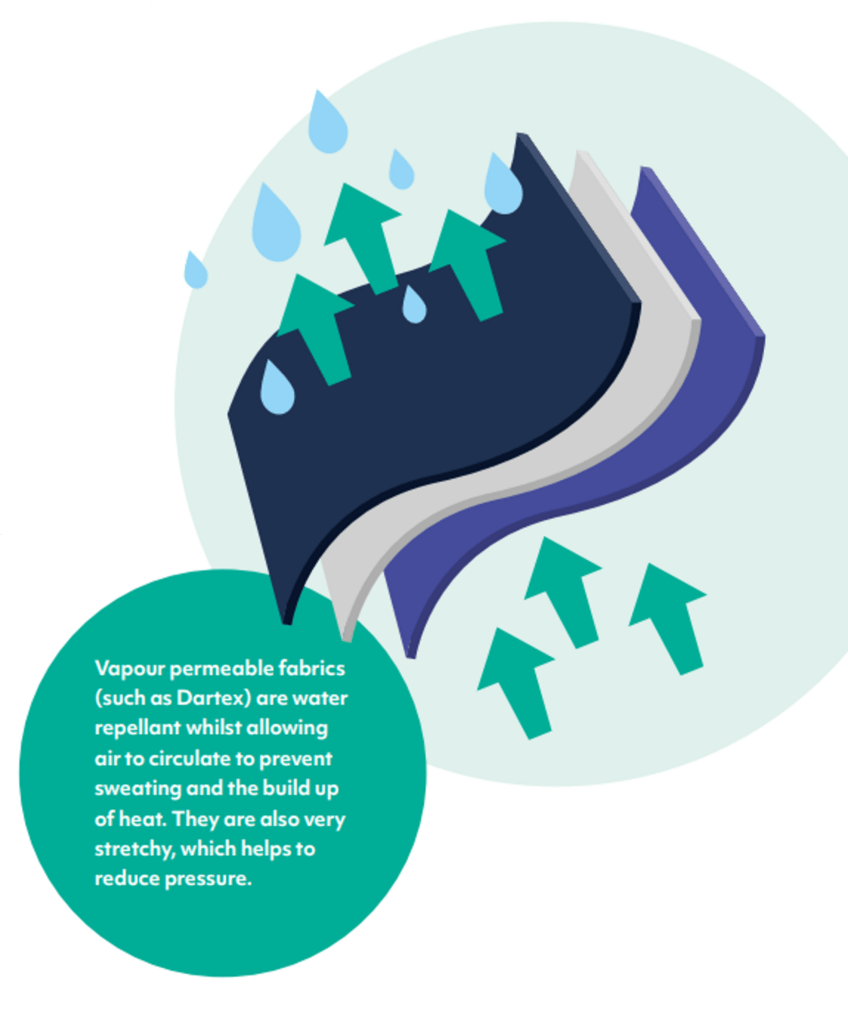
Properties of vapour-permeable fabric
Positioning and Tilt-in-Space
The right positioning features in the chair are key to redistributing pressure evenly over the body, changing the patient’s position to prevent the build up of pressure in any particular area.
Fundamental to this is the tilt-in-space function, incorporated in all our rehabilitation seating, which tilts the patient back in the chair at the same seat angle, to shift the patient’s centre of gravity and spread contact pressure from the thighs and buttocks over a greater area of the body. Backrest recline, incremental tilt-in-space and articulating footrests are additional positioning features we use to give further scope for altering positioning and giving the patient maximum levels of comfort. We provide a range of positioning accessories such as high-level head supports that can be added to the chair to enhance support.

Tilt-in-space functionality
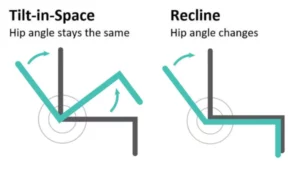
The difference between Tilt in Space & Back Angle Recline
Pressure Cushions
Standard seat cushions in our range would normally be a medium-risk visco foam, but we offer a range of upgrade options such as gel cushions or alternating air to give extra support to high-risk patients with poor tissue viability.
The Role of Beds and Mattresses in Pressure Care
Being bed-bound gives a patient the highest chance of pressure sores, so it is critical that these patients use the right kind of bed and mattress to negate this risk as much as possible.
Profiling Beds
Electric beds such as our Opera range incorporate a profiling action that moves the mattress to align with the patient’s natural body profile, with separate leg and backrest sections. This helps redistribute pressure around the body, preventing any build up from just lying in the same horizontal position.

Opera Solo Profiling Floor Bed
Positioning Aids
Different positioning aids like backrest wedges can help provide a more natural body profile, but the high-spec electric action should remove the need for extra accessories, as the positioning requirements are all incorporated in the electric action.
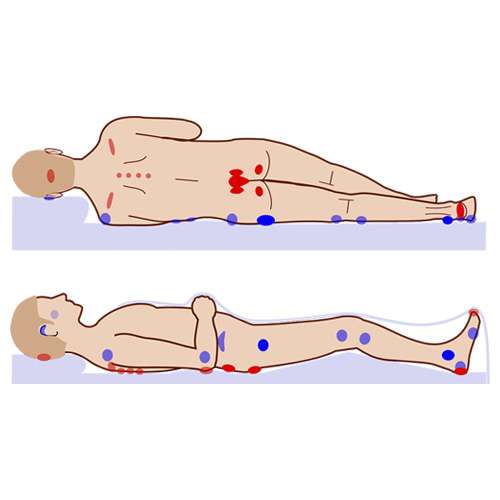
Prone Positioning
Sometimes patients need to be placed in a prone position (face down) if they have surgical wounds on the rear of their body. Some electric profiling beds can facilitate this with trendelenburg and anti-trendelenburg action. Small but frequent changes in position should be performed when in a prone position, due to the high number of sensitive pressure points on the front of the body. This helpful article has a lot of tips for pressure care in this position.
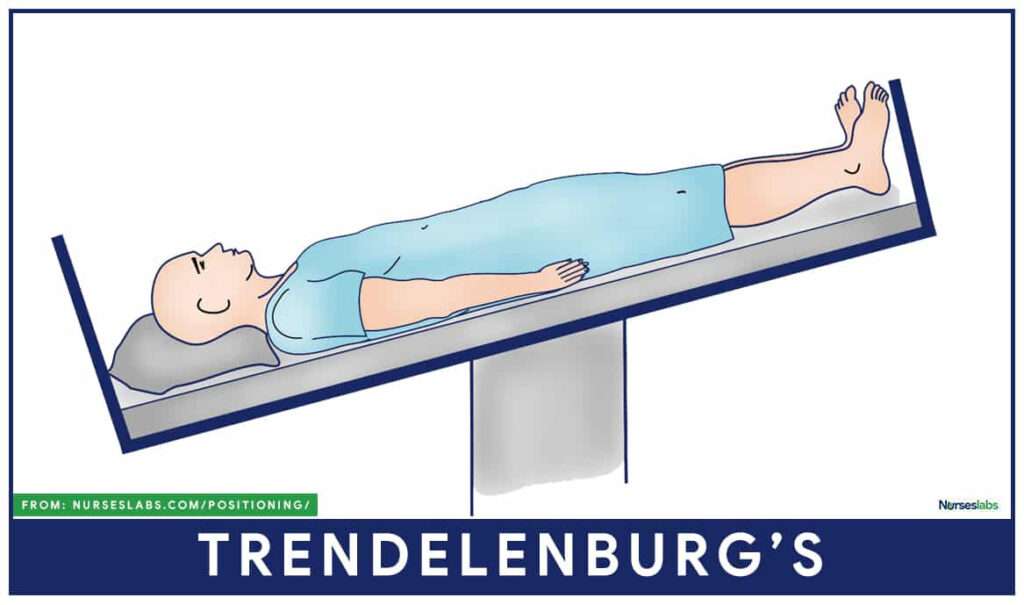
Trendelenburg position
Anti-trendelenburg positioning (patient lain flat with feet higher than head) is used to assist blood circulation.
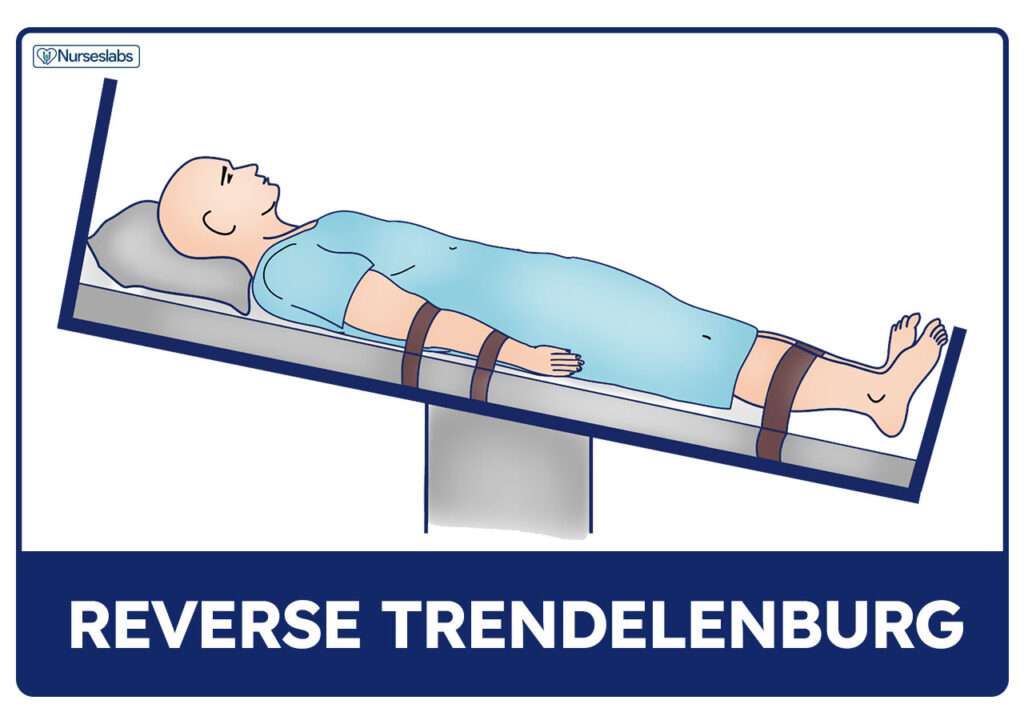
Anti-Trendelenburg position
Mattress Technologies
In-built pressure relief systems like alternating air feature in our mattress range, where rows of air cells alternately inflate to distribute pressure on the skin as evenly as possible.
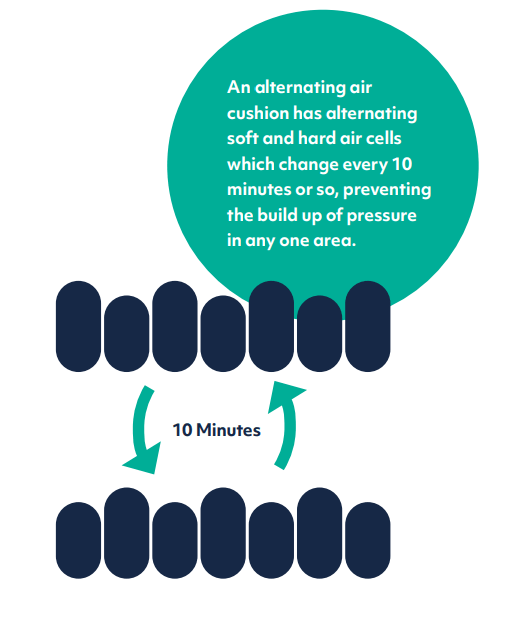
Alternating Air system
Hybrid mattresses combine foam and air, the foam in the air cells helping to absorb some of the noise and vibration from the pump.

Cross-section of a hybrid mattress
Pressure mapping is an advanced technology used to map pressure points on a patient’s body, by using a pressure-sensitive mat linked to a digital pressure map displayed on a screen.
Read our other article to find out more about how air pressure mattresses work.
Prevention Strategies
Holistic Strategies
SSKIN is a useful mnemonic to cover the essential points in pressure care, it stands for:
Surface — make sure your patient is in contact with the right surface
Skin — regular inspection helps detect pressure sores early on
Keep them moving
Incontinence — moisture helps pressure sores develop, ensure your patient is kept clean and dry
Nutrition/Hydration — make sure your patient is eating the right diet and drinking plenty of fluids
Early Mobility to Prevent Deconditioning
The importance of early mobility to prevent deconditioning cannot be underestimated. Delays in getting patients mobilised and discharged from hospital can be very detrimental, resulting in physical problems like poor balance, reduced muscle tone, hypotension, and the inevitable pressure ulcers.
We have developed a range of rehabilitation products designed to get patients back on their feet as early as possible.
Our Rehabilitation Chair improves recovery outcomes with lots of different sitting and lying positions, and a very supportive sit-to-stand function that helps the patient get to their feet as smoothly as possible.

Rehabilitation Chair
The StairTrainer improves physiotherapy programmes, providing a mobile, supportive step-training tool with step height that can be tailored to the individual.

The StairTrainer
Other Pressure Care Campaigns and the Work They Do
Stop Pressure Ulcers
A global network of campaigners that hold events around the world, running promotional campaigns to raise awareness and influence policy makers. They rely on an active network of volunteers and make promotional material free to anyone who wants to support this worthy cause. Stop Pressure Ulcers Day is held on 16th November 2023.
Stop the Pressure Week
This is held 13-17 November 2023, the Tissue Viability Society collaborates with NWCSP, supported by industry organisations, highlighting that pressure care is the job of every clinician in healthcare.
Summary
Prevention being better than cure has never been truer than in the case of pressure ulcers. Many organisations are working together to publicise the critical need for robust prevention practices, so that pressure wounds can be averted at the earliest stages.
For more pressure ulcer prevention strategies, contact our Acute Care team.
Speak To Our Acute Seating Team