Pressure wounds, also known as pressure ulcers or bedsores, are a common and potentially serious condition for people who spend long periods of time in a chair.
These sores occur when there is constant pressure on a particular area of the skin, reducing blood flow and leading to tissue damage. They can be painful, difficult to heal, and even life-threatening in severe cases.
As a specialist seating company, we understand the importance of providing comfortable and effective seating solutions to manage complex health conditions, including the prevention and treatment of pressure wounds.
In this post, we will provide you with a guide on how to prevent and treat pressure wounds in a chair.
Seating Solutions with Pressure Care
Jump straight to…
Preventing Pressure Wounds in a Chair
Prevention is the most effective way to avoid the pain and discomfort of pressure wounds. To prevent pressure wounds from developing, it is important to understand the risk factors and take preventative measures.
Individuals who are immobile, have limited mobility, or have a medical condition that affects their skin integrity, such as diabetes, are at a higher risk of developing pressure wounds. Other risk factors include poor nutrition, dehydration, and incontinence.
Implementing preventative measures such as regular repositioning, utilising pressure cushions, maintaining proper nutrition and hydration, and exercising regularly can significantly reduce the risk of pressure wounds.

In this post, we will discuss the importance of pressure wound prevention, risk factors, and preventative measures that can be taken to reduce the risk of pressure wounds. We will also provide tips for identifying and treating pressure wounds if they do occur.
By understanding pressure wound prevention and taking proactive steps to maintain health, individuals can prevent the development of pressure wounds and maintain optimal health.
Here are some tips to help prevent & manage pressure wounds in a chair:
Regular Patient Repositioning
Changing positions is essential in avoiding pressure sores. It is crucial to change seating position frequently to reduce the amount of pressure on any one area of the body. Repositioning every 15 to 30 minutes can help to keep the blood flowing and reduce the risk of pressure wounds.
Regular repositioning is an essential part of pressure wound prevention and treatment. and can help to prevent pressure wounds from developing or becoming more severe. It is also an effective treatment for existing pressure wounds, as it reduces the pressure on the affected area and promotes healing.
By combining regular repositioning with other pressure injury prevention techniques, such as proper nutrition and hydration, use of pressure redistribution cushions, and exercise, the risk of pressure wounds can be significantly reduced.
Pressure wounds can develop quickly and become severe, causing significant pain and discomfort, but repositioning can help to reduce the risk of skin damage and promote healing.
By using pressure redistribution cushions and repositioning the body every 15 to 30 minutes, the amount of pressure on any one area can be reduced, allowing the blood to flow more easily and preventing skin damage.
Repositioning when seated:
When seated in a chair for an extended period, there are specific areas of the body that are more prone to pressure wounds, including the tailbone, hips, and heels. Repositioning involves shifting the pressure away from these areas and onto different parts of the body, distributing the weight more evenly across the seating surface.
Repositioning can be done in several ways, including shifting weight from side to side, leaning forward, or using a tilt-in-space chair that allows the user to adjust their position easily.
Chair Movements Can Provide Pressure Injury Relief
Chair movements in healthcare seating are instrumental in preventing and treating pressure injuries. These movements offer various benefits that can help minimise the risk of pressure-related damage.
Tilt in Space:
Tilt-in-Space (TiS), as mentioned previously, enables the occupant to be tilted forwards or backwards in a chair whilst maintaining the angle of the knees and hips. This spreads pressure across a greater surface area and prevents the person from sliding out of the chair
Back Angle Recline:
Back Angle Recline (BAR) enables a resting or napping position, or allows the back angle to be increased for those who have fixed hip positioning. Imagine the regular recline that you might find on a sofa or chair at home.
Our assessors often set this to the correct angle on chair delivery, and then disconnect the lever to prevent carers altering it, as moving the backrest angle can increase shear and reduce comfort and support.
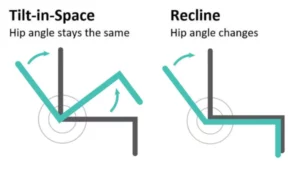
The difference between Tilt in Space & Back Angle Recline is in the hip angle they create.
Automatic Tilt:
If a patient is at particular risk of pressure damage, automatic tilt is available on some electric action care chairs. This continuously changes the angle of the tilt-in-space mechanism, stopping a build-up of pressure occurring in any one area.
Need A Chair With In-Built Pressure Care?
Managing Pressure Injuries with Correct Chair Fabrics
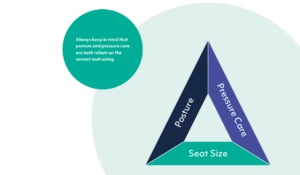
If the person sitting in the chair for long periods of time is at risk of pressure sores, the types of pressure relief fabrics being used in their chair may need to be considered.
Visco Seat Wrap: Medium to low pressure relief
When the risk of pressure injuries is medium to low, our assessors usually prescribe a 2” Visco memory foam is used for the seat wrap, providing extra comfort.
Gel Seat Wrap: Medium to high pressure relief
For situations where medium to high pressure relief solutions are needed, gel-based pressure relief is used for the top 2” of the seat and legrest. These are the areas of the body that have the highest rate of contact with the chair and therefore most likely to develop pressure injuries if left untreated.
Drop-in Seat:
This design allows for a full depth pressure relieving seat cushion (such as a gel or an alternating dynamic air cushion) to be used.
Different prescribed pressure relieving products can be used as pressure care needs change, and optimum pressure relief is given as there are minimal surfaces between the pressure product and the sitter.
Covered Drop-in Seat:
Similar to the drop-in seat, but maintaining the look of a standard chair, the Covered Drop-in has an additional Vapour Permeable or Panvelle Stretch fabric layer between the pressure cushion and the seated person.

Vapour permeable fabrics allow moisture to pass though and keeps both the surface are and the skin dry and less at risk of pressure injury.
Pressure Redistribution Cushions for Wound Care
Pressure redistribution cushions are also an important component of wound care for those who spend long periods of time in a chair.
These wound care cushions are designed to evenly distribute body weight across the seating surface, they can help to reduce the pressure on bony prominences and prevent the development of pressure wounds.
By using pressure care cushions for parts of the body that are at most risk of developing pressure wounds, the risk of pressure wounds can be reduced, and existing wounds can be treated effectively.
They are designed to support the body’s natural shape and prevent the build-up of pressure in specific areas that are prone to pressure wounds, such as the tailbone, hips, and heels.

Alternating Air Cushions are used for patients at the highest risk of pressure injuries.
When selecting a pressure redistribution cushion, it is essential to consider the individual’s needs and preferences. Different materials, such as foam or gel, provide varying levels of pressure redistribution and support. Cushions for pressure injury prevention may come with additional features, such as moisture-wicking fabric or adjustable straps.
It is also important to consider the cushion’s size and shape, as well as the dimensions of the chair, to ensure a proper fit. A cushion that is too small or too large can cause discomfort and may not provide adequate pressure relief.
Gel cushions for wound care and foam cushions for pressure redistribution are common types of cushions used for pressure sore prevention and pressure wound management.
Managing Pressure Wounds with Air
Utilising these cushions in conjunction with other pressure injury prevention techniques, such as repositioning every 15 to 30 minutes, maintaining proper nutrition and hydration, and exercising regularly, can significantly reduce the risk of pressure wounds and promote optimal health.
The Benefits of Pressure Relief Cushions
When combined with proper nutrition and hydration, exercise, and other pressure injury prevention techniques, the use of pressure redistribution cushions can help to promote optimal health and prevent pressure wounds from developing or becoming more severe.
- Proper Nutrition and Hydration: Proper nutrition and hydration are essential in maintaining healthy skin. A well-balanced diet and adequate water intake can help to keep skin hydrated and less prone to injury.
- Exercise: Regular exercise can help to improve blood flow and reduce the risk of pressure wounds. Even simple exercises, such as stretching, can help to keep the body healthy and prevent the development of sores.
Treating Pressure Wounds in a Chair – a Quick Guide
If pressure wounds do occur, it is important to seek treatment as soon as possible. Here are some tips for treating pressure wounds in a chair:
- Clean and Dress the Wound: Keeping the wound clean and covered is essential in promoting healing. Use a mild soap and water to clean the affected area, and apply a sterile dressing to protect it from further damage.
- Reduce Pressure on the Affected Area: Removing pressure from the affected area is critical in promoting healing. This can be achieved by using a pressure redistribution cushion, changing seating position or adjusting the recline of the chair.
- Manage Pain: Pressure wounds can be very painful. Proper pain management is essential in promoting comfort and facilitating healing. There are many over-the-counter and prescription pain relief options available that can help to reduce discomfort.
- Seek Professional Medical Help: If pressure wounds are severe, it is important to seek medical attention. A healthcare professional can assess the severity of the wound and recommend appropriate treatment options.
Conclusion: Caring for Pressure Wounds in a Chair
Pressure wounds can be a significant concern for people who spend long periods of time in a chair. However, with proper prevention and treatment, they can be avoided or managed effectively.
By regularly repositioning, using pressure redistribution cushions, maintaining proper nutrition and hydration, and exercising, you can reduce the risk of developing pressure wounds.
If pressure wounds do occur, prompt and appropriate treatment can help to promote healing and prevent further damage. This is why, at Vivid Care, we design all out seating solutions to help prevent and manage pressure injuries when sitting in a chair. Contact us today to find out how our specialist seating solutions can improve patient outcomes for your healthcare facility.
Speak to our team today
Frequently Asked Questions (FAQs)
How can I prevent pressure sores while sitting?
To prevent pressure sores while sitting, follow these tips:
- Reposition yourself every 15 to 30 minutes to relieve pressure.
- Use pressure-relieving cushions designed to distribute weight evenly
- Ensure proper hydration and maintain a balanced diet to support skin health
- Check your skin regularly for any signs of pressure sores, such as redness or irritation
What is the best cushion for pressure sores?
The best cushion for pressure sores varies depending on individual needs. Common options include:
Gel cushions: These provide even distribution of weight and reduce friction.
Air cushions: These adjust to your body’s shape and are good for continuous pressure relief.
Foam cushions: High-density foam cushions provide firm support and are ideal for those who require stability. Consult a healthcare professional to determine the best cushion for your specific needs.
How often should I reposition to prevent pressure ulcers?
It is recommended to reposition yourself every 15 to 30 minutes while sitting to relieve pressure and improve circulation. Frequent movement helps prevent pressure sores by distributing weight across different areas of the body.