Prescribing specialist seating for clients with spinal cord injuries can be incredibly difficult. The phrase ‘spinal cord injury’ is an umbrella term that covers a wide variety of conditions, which in turn, covers a wide variety of presentations and issues. This includes paraplegics (paralysis of legs only) and quadriplegics (paralysis of legs and arms). A group of people with spinal cord injuries could have completely different levels of mobility and needs, which means we can never use a cookie-cutter approach to clients with spinal damage.
Nevertheless, spinal cord injuries can be catered to with the right seating. Once you have identified your client’s condition, it will become much easier to find a chair that fits their needs. Here is our guide on how to find comfy seating for people with spinal cord injuries.
Jump straight to…
What is a spinal cord injury?
It might sound like a simplistic answer, but anything that causes damage to your spinal cord is classed as a spinal cord injury (SCI). This includes fracturing or moving vertebrae, which can damage the nerves. Depending on where the injury is in your spinal cord, it could cause anything from tingling and a loss of sensation to paraplegia or quadriplegia.
The spinal cord is a super-highway for the body’s nervous system, meaning that any injury could be life-changing.
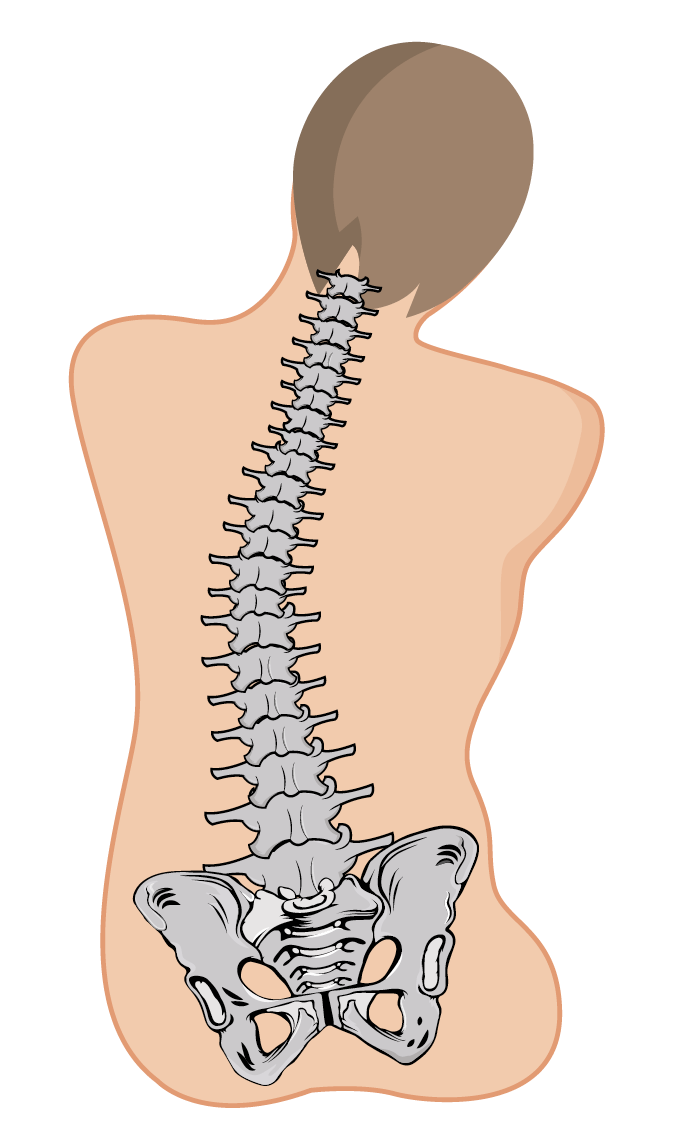
The spinal cord has an incredibly important function in the body — it carries your central nervous system from the base of your brain right down to your lower back. It’s the main route the carry messages throughout your body. This allows us to move, feel pressure or heat, and carry out fundamental functions like breathing.
Your spinal cord is about the width of your little finger, so an SCI can easily become life-changing. Spinal cord damage means that the messages between our body and brain are interrupted, or simply cannot get through. This can result in a loss of feeling or mobility below the level of the SCI.
Sections of the spine
Whenever healthcare professionals talk about the spine, they split it into four sections:
- The cervical spine (C1 — C8) runs through your neck and ends around parallel with the tops of your shoulder blades.
- The thoracic spine (T1 — T12) then continues from the shoulder blades throughout your chest to the base of your rib cage.
- Your lumbar spine (L1 — L5) picks up beneath the rib cage and ends the top of the pelvis, covering your lower back area.
- And finally, the sacral spine (S1 — S5) is fused and covers your sacrum and pelvic area.
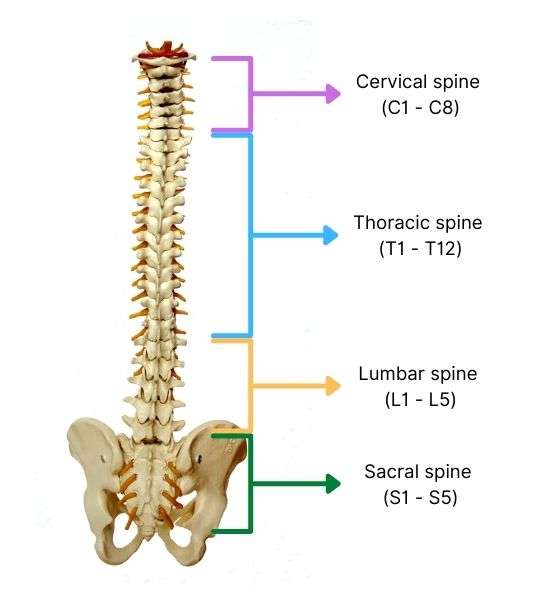
The spine is split into four sections; cervical, thoracic, lumbar, and sacral.
Any SCI will be referred to with letters and numbers. These correspond with the position of the spinal cord damage. For instance, if you have a T6 SCI, then the damage has been sustained in the middle of your thoracic spine. If you have an L1 SCI, then the injury will be at the top of the lumbar spine.
Terminology of spinal cord injuries
The spine is a very complex system within the body, so it often comes with very specific terminology. SCIs can be ‘traumatic’ and ‘non-traumatic’, or ‘complete’ and ‘incomplete’. These also give extra context to an SCI that’s valuable to know. Given that the spine is broken up into different sections and numbers, there is a wide variety of SCIs that can occur to different degrees.
Traumatic or non-traumatic SCI?
This tells us whether the SCI was caused by a traumatic event or not. A traumatic SCI would be caused by something like a fall or a car crash, whereas a non-traumatic SCI would cover things like spinal degeneration, surgical complications, or a stroke.
Complete or incomplete SCI?
Complete and incomplete tells us what level or type of SCI has been sustained. If there is no voluntary movement or feeling from the site of the injury and below and both sides of the person’s body are affected, then the SCI is complete.

If an SCI is complete, then the person will have no sensation below the injury site. If the SCI is incomplete, the person may still have some sensation and mobility.
If there is some sensation (i.e., in the bladder and bowels), and the person still has some movement below their injury site, then the SCI is incomplete.
What is the difference between paraplegic and quadriplegic?
Paraplegia and quadriplegia refer to the amount of immobility and loss of sensation following an SCI. Depending on where the SCI is, a person may lose feeling and mobility in just one area or totally from the neck down.
Paraplegic means that the person has lost feeling and movement in both legs and occasionally, part of the lower abdomen.
Quadriplegic means that all four limbs have been affected and sometimes areas of the chest, abdomen, and back.
Different types of spinal cord injuries
Here is a guide to different SCIs, although it’s important to note that symptoms and presentations in clients can still vary.
Cervical nerve injuries (C1 — C8)
SCIs that occur in the cervical spine (neck) can often cause some of the most severe spinal damage. Due to the level of the injury, SCIs around the cervical nerves can affect all four limbs and may prevent the person from being able to breathe, cough, or swallow independently. Some injuries may affect the person’s ability to speak.
Any injuries to the C1 — C8 area will put the phrenic nerve, radial nerve, median nerve, and ulnar nerve at risk. These nerves cover your arms and part of your upper back.
Injuries like a C4 complete, broken C3, or a cervical cord contusion (where some of the spinal cord is crushed, but the fibres and tissues attached to it remain intact) can result in quadriplegia or reduced mobility and sensation in the arms and upper back.
The lower down the spinal cord the injury is, then the lesser the damage might be. If the SCI is in the low-cervical nerves (C5 — C8), then the person may retain some mobility in their upper arms and elbows, but they are likely to have some level of paralysis in their wrists or hands.
People with C7 or C8 injuries may still be able to flex their wrists and fingers to a degree and may have regular movement in their shoulders. They may still be able to grip items with their hands and can possibly drive an adapted vehicle.
Thoracic nerve injuries (T1 — T12)
As the thoracic area covers more of the spinal cord, it is more common for SCIs to be in the T1 — T12 vertebrae. SCIs here are less likely to affect a person’s arms (although it can still happen). SCIs in the thoracic spine could affect nerves leading to the lower body, like the femoral never or the sciatic nerve.
Injuries between the T1 and T5 vertebrae could affect some sensation and movement in the person’s chest, abdomen, and mid-back, but their arm and hand function should still be normal. People with an SCI in their upper thoracic nerves can usually use a manual wheelchair or even stand in a standing frame for a length of time. However, they may need extra support to hold themselves up straight when seated.
SCIs in the lower thoracic nerves (T6 — T12) may affect trunk muscles, but they could have better control over their balance and abdomen when seated. If their SCI isn’t too severe, they should be able to cough on their own.
As the injury is lower in the spine, their upper body function should be usual, meaning that they are paraplegic. They might also be incontinent due to loss of sensation in the bladder and bowel.
Lumbar nerve injuries (L1 — L5)
As this is one of the lowest parts of the spine, the level of spinal cord damage in this area should not be as severe. That being said, the person’s control over their bladder and bowel may still be inhibited.
SCIs in this area may result in a loss of function and sensation in the hips and legs, but the individual may still be able to walk with mobility aids.
Sacral nerve injuries (S1 — S5)
This is the lowest part of the spine before we hit the coccyx, but injuries can still be life-changing in this area. SCIs in the sacral nerves could lead to less function in the hips and legs and some degree of incontinence. However, the individual may still be able to walk.
Seating issues for people with SCIs
Since the degree of SCIs can vary so much from person to person, there is no singular approach you can take when finding specialist seating for someone with spinal cord damage, quadriplegia or paraplegia. When carrying out your seating assessment, it’s integral to factor in the details of the SCI — specifically the location of the SCI in the spinal cord and if any level of mobility/function has been retained.
Poor pelvic positioning and pelvic obliquity are a concern in seating for people with SCIs.
You will need to create a bespoke solution for your client to ensure that their postural needs and comfort have been catered to. For clients with SCIs, you might find the following common seating issues:
– Poor postural control: Given the client’s reduced muscle function, they may not be able to hold a healthy midline position along the spine, which compromises their postural control.
– Scoliosis or kyphosis: Caused by the person’s poor postural control, kyphosis and scoliosis may be caused by the client’s inability to hold a healthy position with the spine.
– Pelvic instability or poor pelvic positioning: The client may slouch (posterior pelvic tilt) or have pelvic rotation or obliquity caused by loss of muscle function in the lower body.
– Contractures: For individuals with little to no muscle function in their legs, contractures may cause severe discomfort and pressure injuries if not catered to with specialist seating.
– Uneven muscle tone: Some clients may have more function on one side of their body, or they may have more function and muscle tone in their upper body. A typical chair might not be comfy or supportive of their needs.
– General fatigue: As with any condition, fatigue can also be a big problem for someone who is seated for most of the day. Having a chair with flexible positioning and mobility could make all the difference.
Given the variety of presentations and needs a client may have, your seating solution will need to combine an array of fixtures and features that will cater to the client’s individual needs. (For further information on seating issues, please see our free Specialist Seating eBook.)
The best chair for spinal cord injuries
To tick all the right boxes for your client, a flexible seating system is your best bet. Particularly for people with SCIs, you will need a chair that can be changed and adjusted to meet their needs over a longer period. The type of chairs you should be looking at will depend on whether your client is hoisted.
Chairs for people who are hoisted
We often recommend care chairs for clients that are hoisted. This is because care chairs tend to offer more positioning options and an extra level of support.
The Lento care chair features an adaptable seating system that can be altered as the client’s needs change. It features adjustable seat width, height, and depth to make sure that the individual’s postural needs are catered to. This makes it the ideal option for someone with an SCI who is hoisted.

The Lento care chair is the best seating option for someone with an SCI who is hoisted.
You can choose between a waterfall and cocoon backrest depending on the individual’s postural needs and the level of their SCI. The Lento care chair also features a backrest and legrest recline along with tilt-in-space as standard to ensure the client is always comfortable.
Chairs for people who are not hoisted
For a client who is not hoisted, then you might not need the same level of support. If that is the case, then we would recommend you look at rise and recline chairs instead — specifically the Lento rise and recline chair with wheels. The Lento riser recliner can be repositioned as necessary and feature the same adjustable seating system, meaning that the client’s needs can be catered to over time should their condition change.

For someone who has an SCI and does not require hoisting, then the portable Lento Mobile Rise & Recline chair is your best bet.
The backrest cushions can also be swapped out to provide support as needed. For clients with more severe postural needs, you might opt for extendable wings or a cocoon backrest. Like the care chair option, the Lento rise and recline can also be adjusted in terms of positioning.
Conclusion
Finding comfortable, supportive seating for people with spinal cord injuries is a must, and there are plenty of articles detailing the importance of postural support in managing SCIs. The key is to approach each client’s needs separately due to the varying nature of SCIs.
SCIs can range in their complexity depending on where they are in the spinal cord itself, so it’s important to assess your client’s postural needs and abilities before you prescribe any specialist seating. But it is always worth bearing in mind that flexible seating solutions will offer more support in the long run, helping you to manage any changing needs your client may have.














