Introduction
Winter peaks put a strain on the NHS each year. One of the key focuses for the NHS in 2023 is to reduce variation in acute frailty service provision and improve recognition of cases that could benefit from specific frailty services and ensuring referrals to avoid admission.
Frail patients are particularly vulnerable during winter pressure peaks. They are more likely to experience complications from seasonal illnesses, such as influenza and norovirus, and they may have difficulty coping with the cold weather.
It is important to ensure that frail patients are comfortable and well-supported during this time.
NHS Long Term Plan for Frailty Patients:
The NHS Long Term Plan (agreed in the 2018 government budget) acknowledges that services are not joined-up or responsive enough to the needs of older people with frailty and looks to fix this by offering more support to help older people stay at home independently for longer.
The NHS Long Term Plan includes three new service models:
- Improve NHS care in care homes.
- Identify & provide proactive support to older people with frailty in the community.
- Enhance rapid crisis response in the community
Enhanced Health in Care Homes:
The Long Term Plan aims to implement the Enhanced Health in Care Homes (EHCH) model across care homes in England by 2024.
The EHCH model promises to ‘upgrade NHS support to all care home residents by 2023/24 by moving to a more joined-up, collaborative approach’ that will include:
- Health & Social care
- Voluntary & Community Services
- Social enterprise (VCSE) sector
- Care home partners.
This new model of care provision will offer more proactive, person-centred care that considers the needs of older people, their families and care home staff as opposed to the traditional reactive care model.
Under EHCH, older people living in care homes should expect the same level of support as if they were living in their own home.
Enhanced Health in Care Homes Means That Older People in England Can Expect:
- Named general practice support
- Timely access to emergency out of hours support
- Access to regular clinical pharmacist-led medicine reviews
- Support for care homes to share information relevant to residents’ care.
Urgent Community Response (UCR):
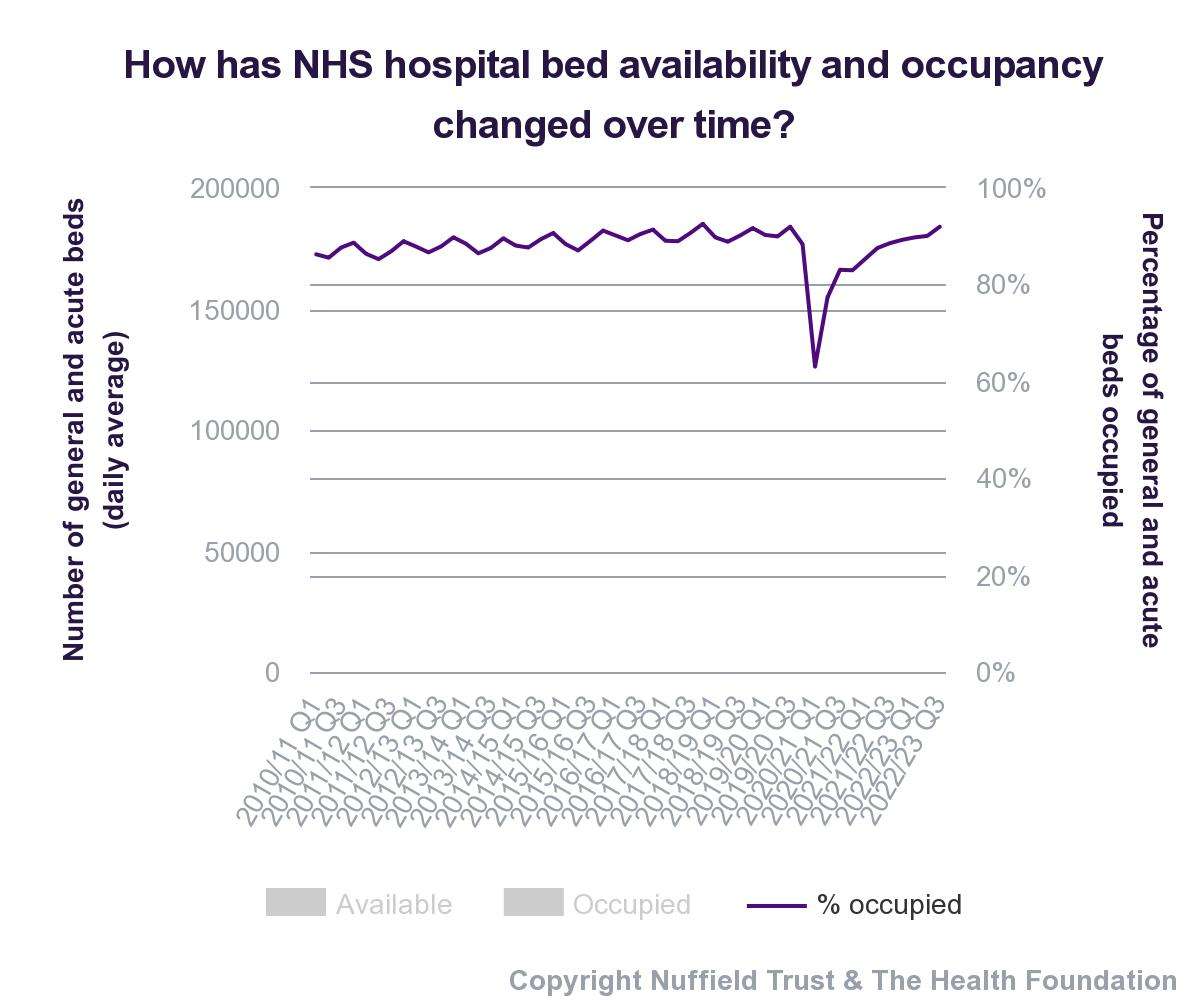
The NHS Long Term Plan will look to increase the volume and accessibility of NHS community and intermediate health packages to help free up over one million hospital bed days.
Older people in England find they are admitted to the hospital and find themselves staying in the hospital for longer periods of time than they would have expected.
Too often, these older people stay in hospital for longer than they should or have to simply due to a shortage of services in the community that could support them at home.
During winter pressures, hospitals can find themselves overwhelmed with patients because of:
- Increases in admission
- Delayed patient discharge
The aim of the EHCH model is to make sure that older people have urgent access to:
- GPs
- District nurses
- Mental health teams
- Allied health professionals — such as physiotherapists
As it is, older people too often find themselves waiting for weeks or even months for health support after an illness, injury or operation.
This has real life consequences beyond making a person wait, opportunities to regain function and independence are lost because people can’t access the rehabilitative equipment that they need.
Patient discharge delays can also mean that older people remain stranded in hospital, increasing the chance of cross-infection.
To reduce the risk of hospital admission The EHCH aims to provide access to these services within two days of referral.
Community Teams
Community health teams provide support to people with complex health and care needs to live independently in their own home for as long as possible.
Services also include health promotion services such as school health services and health visiting services.
There are a lot of community health services, most relevant for older people with frailty are:
- Urgent Community Response (UCR) including 2 hour rapid crisis response services
- Community occupational therapy, physiotherapy & speech and language therapy
- Specialist nurses (diabetes, COPD, heart failure, incontinence, tissue viability)
- Bed-based community rehabilitation & Falls prevention services
- Wheelchair services & Home health visiting
- Community end of life and palliative care
- Community physiotherapy & Musculoskeletal therapy
- Pulmonary or cardiac rehabilitation
- District nursing
What is Frailty?
The NHS defines frailty as “being less able to cope and recover from accidents, physical illness or other stressful events” and notes that it should be treated as a long term condition throughout adult life.
Frailty (instead of age) is an good way of identifying people who may be at greater risk of:
- Future hospitalisation
- Care home admission
- Death
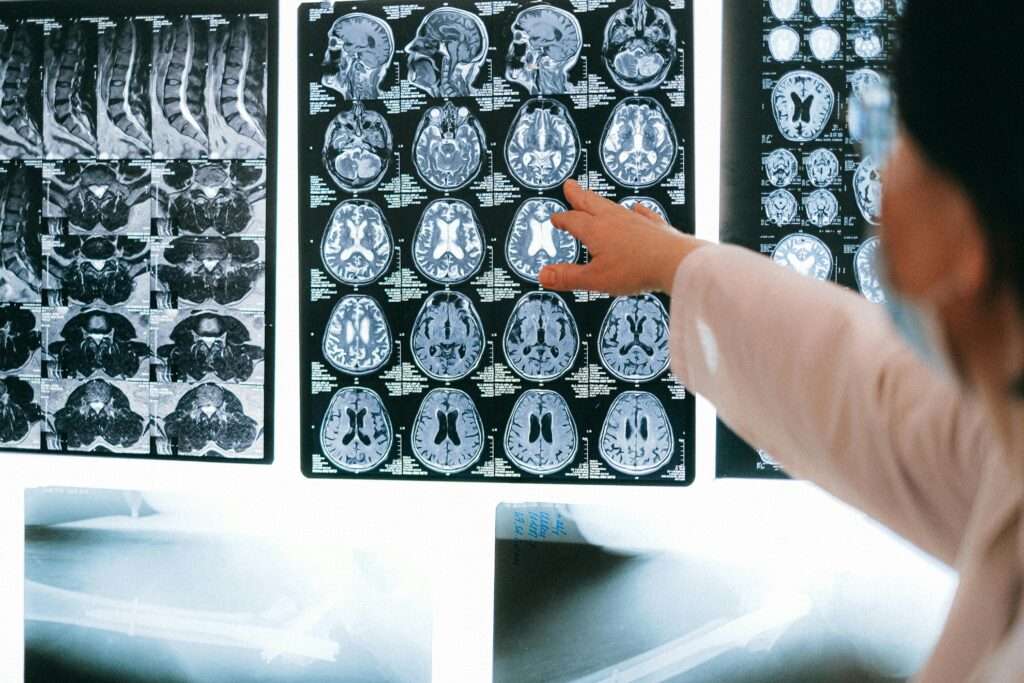
Older people with frailty who need to undergo surgery can have less successful outcomes if the frailty has not been identified prior to the operation.
The Long Term Care Plan aims to tackle frailty in the community with:
- Prevention
- Early identification
- Ongoing appropriate support
The Plan also pledges to improve access to recovery, rehabilitation and reablement support including care rehabilitative packages.
At the moment, older people often experience long waits for support such as rehabilitative care package. These packages are recommended after an assessment by a healthcare professional and can include:
- Home adaptations
- Mobility Equipment (riser recliners & profiling beds)
- Help after coming home from hospital
- NHS continuing healthcare
- Nursing in a care home (NHS-funded nursing care)
Increased access to the right healthcare packages after an episode in hospital can greatly increase the chances of quality recovery for an older person with frailty.
By 2024, the Plan aims to make sure older people with frailty people are able to access help within 2 hours of being referred.
Summary:
Winter peaks put a strain on the NHS, especially for frail patients who are more vulnerable to complications. The NHS Long Term Plan aims to improve care for frailty patients by offering support in care homes, proactive support in the community, and enhanced crisis response. The plan also includes the implementation of the Enhanced Health in Care Homes (EHCH) model and urgent community response (UCR) to provide timely access to healthcare services.
Community teams play a crucial role in supporting people with complex health needs, and the plan focuses on prevention, early identification, and ongoing support for frailty.
Initiatives outlined in the Long Term Plan:
- Improving access to healthcare packages
- Reducing wait times
- Facilitating efficient patient flow in hospitals
The plan from the NHS aims to enhance recovery and independence for older people with frailty, reduce hospital admissions, improve the quality of care, and enhance the overall well-being of older people with frailty.
These efforts are crucial in ensuring that frail patients receive the support and assistance they need, especially during winter peak periods.