Speeding up patient discharge is a critical priority for the NHS in the wake of the pandemic. Bed occupancy in NHS wards reached a staggering 94% in November 2022, putting immense strain on inpatient wards and resulting in higher waiting lists.
The shortage of hospital beds following the pandemic is clearly a major factor in this, but where space is at a premium and budgets are stretched, helping to speed up discharge will make a big difference to the capacity issue.
Jump straight to...
Causes and Implications of Slow Discharge Rates
To free up discharge, an analysis of the factors contributing to delays is needed.
Deconditioning
Patients who undergo surgery need a reablement program to get them back on their feet as soon as possible. If rehabilitation is not started early enough, the patient’s condition can deteriorate and result in pressure sores, poor balance and muscle tone, and hypotension.
This creates a vicious cycle as the patient then needs further treatment before they are well enough to be discharged.
Bed Blocking
The number of patients in hospital that are medically fit to be discharged has risen dramatically, currently sitting at around 12,500. This bed blocking is caused by the wrong equipment being available and inadequate community care provision. This has been helped in part by the £500m patient discharge fund released in November 2022, helping care homes buy more beds and increase workforce capacity to receive an influx of discharged patients.
Inadequate Community Care
As already mentioned, this is an ongoing issue as local authority budgets are stretched. If patients do not receive sufficient follow-up care after treatment, particularly after major trauma or stroke, this can lead to re-admission. This is being tackled on multiple fronts, by increasing workforce capacity with the workforce recruitment and retention fund, and virtual wards as covered below.
Insufficient Beds in the Community
Contributing to the bed-blocking issue, this again comes down to insufficient equipment in being available for a person’s home or care home to continue their care plan following hospitalisation.
Insufficient Hospital Beds
Not having enough beds available on the ward has a knock-on effect on A&E wait times, by slowing down admissions from A&E. This puts pressure on the emergency services, as ambulances wait longer to admit patients into overloaded A&E departments.
Increased Waiting Times
In the fallout from the Covid-19 pandemic there has been a massive increase in waiting times for treatments, making the need to speed up patient discharge even more pressing.
The current waiting list for elective treatment stands at 7.42 million, which perhaps is not the true figure due to the hidden list of people who haven’t referred or have had treatment cancelled due to the pandemic.
Ways to Speed up Discharge
Seating Strategies
Having an effective seating program is essential to helping patients through their treatment and recover for discharge. Our Lento seating range is designed to help patients rehabilitate faster. This is due to the following features:
- Size configuration to fit any patient regardless of size, without tools
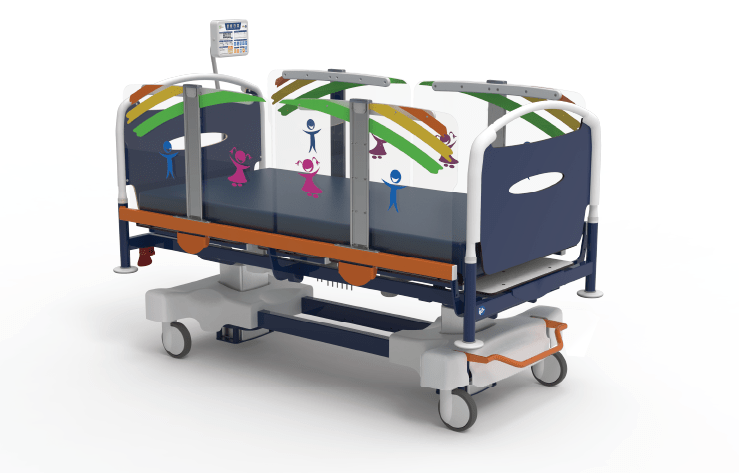
- Paediatric to bariatric range, covering all ages and stages
- Interchangeable parts and accessories, including different backrests and lateral supports
- High pressure relief systems
Virtual Wards
Virtual wards are an innovative strategy introduced to relieve bed capacity inside hospitals, by providing care and support to the patient while they are in the comfort of their own home. Being in their own home and free from the risk of hospital-acquired infections will improve their health and wellbeing even further. Care is provided by a multidisciplinary team who provide tests and treatments, delivering these to the patients home and monitoring their progress remotely via a wearable device.
New Hospital Programme
Boris Johnson promised in 2019 to build 40 new hospitals by 2030. This pledge has been watered down slightly since the health secretary revealed that refurbishments and extensions were included in the magic ‘40’. Nevertheless, this still constitutes a significant capital investment into NHS capacity.
Increasing Workforce Capacity
Increasing the size of the community care workforce has been a recent strategy, backed by the Workforce Retention and Recruitment Fund. This £162.5m fund was designed to help staffing levels over the winter period and boost capacity in social care.
Improving Access to Funding
Getting access to funding is vital for community care organisations to improve their service provision. We are able to assist with this process by helping care groups navigate the funding landscape, as covered in a previous article.
Some examples of recent funding released by government includes:
- £500m discharge fund — the aim of this fund was to reduce bed blocking by allocating 40% to local authorities and 60% to Integrated Care Boards (ICBs).
- £250m hospital discharge fund — released on the back of the £500m fund this was to buy up thousands of beds for care homes to absorb a wave of hospital discharges.
The Role of ICBs
Integrated Care Boards (ICBs) bring together different partners across the health and social care spectrum to share issues and have a coordinated approach to solving problems. This is a major step forward in terms of resolving the discharge issue.
Replacing the old CCG model, they are region-specific so can prioritise the main health and social care needs for their area, whether this be discharges, community beds or social care.
Rehabilitation
Re-enabling patients after a course of treatment is a key driver in reducing discharge times. Often the rehabilitation wards won’t have the right equipment to make this happen. We have a couple of products in our range specifically for this purpose, the Rehabilitation Chair and the StairTrainer.
The Rehabilitation Chair makes recovery easier by providing lots of positioning options to reduce deconditioning and assist with the sit-to-stand process.
The StairTrainer is a mobile step-training tool with a variable step height to tailor to the patient’s level of rehabilitation.
National Discharge Frontrunners
Six healthcare partnerships across the UK have been selected as national discharge frontrunners, each one championing a specific strategy to improve discharge rates. These six strategies are:
- A new data tool to manage service performance (Sussex Health & Care ICS)
- Partnerships between NHS and Social Care to support discharged patients (Warwickshire Place)
- Integrated acute/community team to improve coordination between care settings (One Croydon Alliance)
- Establishing an Active Recovery Service focusing on rehabilitation and reablement (Leeds Health & Care Partnership)
- Dementia hubs to reduce readmission (Northern Care Alliance)
- Innovative use of data and real-time intelligence (Humber & North Yorkshire ICS)
Summary
There is a vast range of strategies being employed across the health and social care spectrum to increase hospital discharges, as we have covered in this article.
If your specific trust is facing a discharge issue we can help, through our knowledge of discharge schemes and equipment solutions.
Contact us for a free consultation