With the NHS waiting list at an all-time high of 7.42m, reducing waiting lists and wait times for elective treatments is hot on the government’s agenda. To provide some context, the waiting list stood at 4.05m at the start of the pandemic.
Over the pandemic period, average wait times for elective treatments doubled, with the national maximum wait of 18 weeks far exceeded. 3m patients have waited longer than 18 weeks for treatment, 12% of these having waited longer than a year.
These numbers don’t include the ‘hidden backlog’ of patients that haven’t referred for treatment either because of infection fears or reluctance to come forward because of the nature of the waiting list. This hidden list is estimated to be at over 10m.
The pressure on elective treatment capacity is an intense crucible of ongoing service pressures, combating the backlog and workforce shortages. Poor patient throughflow is another major factor in this problem, with bottlenecks putting reverse pressure on elective care due to discharge delays.
What is the NHS doing to reduce these waiting times and improve access to elective treatments?
Jump straight to...
NHS Strategy to Reduce Backlog of Elective Care
What is Elective Care?
Elective Care refers to a broad range of non-urgent services in the NHS, e.g. diagnostic tests, scans and cancer treatments. This is nearly always patient-initiated, and introduced into the NHS through GP or consultant referral.
NHS 4-Point Plan
One of the NHS’s headline goals is to completely eradicate waits of over a year by March 2025.
Their strategic plan in delivering this mission is articulated in their 4-point plan released in February 2022, titled “Delivery plan for tackling the COVID-19 backlog of elective care”.
This takes the form of four main sub-strategies:
-
-
-
-
- Increasing health service capacity
- Prioritising diagnostics and treatment
- Transforming the way we provide elective care
- Providing better information and support to patients
-
-
-
1: Increasing health service capacity
Growing the workforce
Health Education England (HEE) have merged with NHS England and NHS Improvement to provide a more centralised coordination of workforce planning. More elementary strategies include addressing staff welfare, with greater sick leave and stress & burnout being reported by operating staff. Greater internal mental health support and welfare services will be provided within the NHS system.
Greater use of AI and automation will be employed to relieve clinical staff of burdensome admin tasks. Staff flexibility will be promoted, allowing multi-skilled staff to work across different functions to manage fluctuation in demand.
Increasing capacity with digital technology
Utilising the power of digital technologies, with tech-supported virtual wards, expanding the NHS App for wider use, and automating tasks for non-clinical work with Robotic Process Automation
Reforming Covid-style Infection Prevention & Control measures
Returning IPC measures to pre-pandemic conditions as closely as possible, as the current stringent measures reduce operating efficiency.
Working more closely with the independent sector
Elective care boards within each ICS (Integrated Care System) bring together the private, public and charitable strands of the healthcare sector. This filters down to the patients, giving them more choice, including access to private healthcare. Transferring high volume and low complexity treatments to the independent sector has been a successful strategy in increasing capacity.
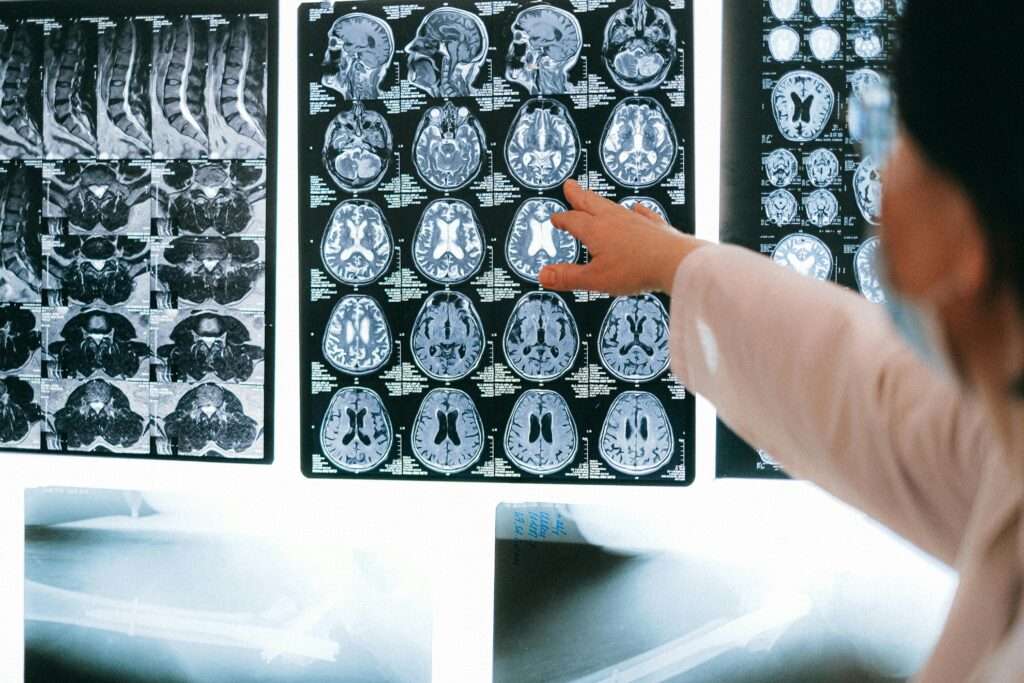
2: Prioritising diagnosis and treatment
Clinical Prioritisation Programme
Building on good practice on the management of waiting lists, including prioritisation frameworks for surgery, diagnostics and endoscopy.
New national network for long waiters
Reviewing patients waiting over 18 months at 3 monthly intervals, to see if their condition has changed or alternative pathways can be offered.
Prioritising cancer referrals
Encouraging quicker testing, with national campaigns such as Help Us Help You.

3: Transforming the way we provide elective care
Expanding diagnostic centres into the community
Making diagnostic services more generally available in the community. We are able to help with deployment of these schemes through rapid delivery and set-up of beds and equipment through our logistics partner Dependall. Our logistics partner assisted the setup of Dorset Health Village, a new outpatient assessment clinic located at the top of a Beales Department Store in Poole.

Breast screening at Dorset Health Village
New surgical hubs
New initiatives like the Theatre Productivity Program have built on the success of surgical cancer hubs. Physically separating elective services in this way from emergency departments helps to preserve capacity within elective care and prevent ‘spill-over’.
Quicker access to specialist advice
Providing direct access from the GP to specialists and consultants helps earlier diagnosis and direct the patient to the right treatment pathway earlier on in the process.
4: Providing better information and support to patients
My Planned Care
An open access web-based platform and an invaluable resource for patients, providing transparency on timescales. This could potentially be integrated into the NHS App, making it more widely available.
Support patients preparing for surgery
Perioperative Care Coordination teams are a mixed group of clinicians to proactively inform and advise patients pre-treatment and provide the support they need.
Expanding and Strengthening the Workforce
Examples of previous initiatives in this area include the Workforce Retention Funding, a government-led funding scheme to address local workforce capacity pressures. We were pleased to support the North East Lincs region, providing single-handed equipment and technologies to free up workforce time and improve patient outcomes.
Championing single-handed care equipment and standardising our seating is one of our key focuses, to help achieve NHS staffing efficiencies, reduce training and equipment downtime and create procurement economies of scales.
Reducing the manual handling burden for staff and preventing repetitive strain is addressed with the VELA chair range, focusing on treatments like mammography screening and radiology. This has been proven to reduce sick days and improve the health of workforce teams.

VELA Mammography chair
The NHS is undertaking a recruitment drive for junior doctors and nurses, and has a bank of over 17,000 reservists it can deploy at short notice to increase capacity.
Mental health support for the NHS workforce has received fresh emphasis, which we have been pleased to support with our tips and advice for managing mental health for healthcare workers.
Investing in digital infrastructure will increase workforce efficiency in areas like pathology, imaging and AI.
Other Pressures on Elective Care
Clearly, winter is a time of increased pressure on our health service, with flu and respiratory infections rising and putting pressure on A&E services. Pressure on A&E causes longer ambulance waits, as experienced in the 2022/23 winter crisis. Our Mobile Day Surgery Chair is designed to speed up A&E admissions, mobilising the patient from point of reception into A&E through to short-term emergency treatment, with multiple positioning options.
The elderly and those with weaker immune systems are more vulnerable to infection at this time of year, and need assistance in the event of a fall if they are less mobile. The ambulance strikes last year had a significant impact on the ability of the ambulance service to respond to category 3 callouts, increasing the need for community support and falls response equipment like the Raizer and HipGuard.
Covid-19 is an existential threat to health service provision, as the successful delivery of the NHS’s 4-point plan relies heavily on Covid rates remaining low. This is something that is difficult to foresee but will involve a far greater understanding of the management of this disruptive virus.
Conclusion
Central to achieving a reduction in waiting times in line with the NHS targets is an increase in service capacity. Increasing workforce capacity and greater utilisation of technology are key strategies to return the NHS to more sustainable levels of service provision.
For more advice and insights on how we are helping the NHS improve access to elective treatments, contact our NHS Partnerships Team.
For more specialist information