Infection — A Global Issue
What is infection control?
Infection and the spread of it is something that has become more engrained in our inner psyche since the advent of Covid-19. However before we get too immersed in visions of face masks and Covid tests, let us take a step back and consider infection control in its proper setting.
Infection control is basically stopping the spread of infection. Now for the hard bit. It’s also known as infection prevention, a preferred term for some as it suggests trying to eliminate the infection rather than just control it. Anyway, more of that later…
Jump straight to...
1.a Why is infection control important?
Bacteria and germs are all around us, but in some environments the risk of harmful bacteria takes on a new dimension and this risk needs to be managed.
In healthcare environments, infection control is evidently a priority. Healthy people build up resistance to antibodies, but patients who have weak immune systems can be more vulnerable to contracting diseases and infections.
Florence Nightingale (a.k.a. “the lady with the lamp”) was the pioneer of infection control in healthcare settings as we know it today. When working in a field hospital on the Crimean War front she observed that men were dying not because of their injuries on the battlefield but from diseases they picked up in the sick bays. By improving ventilation, stopping overcrowding and sterilising equipment, death rates were reduced by two thirds. Thanks to Florence Nightingale and her foresight, the principles of sanitation and sterilisation have become the bedrock of established infection control science today.
1.b How do infections spread?
Harmful bacteria (e.g e.coli) thrive in warm, wet environments, which can build up if contact surfaces are not disinfected regularly.
Viruses are airbourne and spread via moisture and tiny droplets when people sneeze.
Infections spread by the transfer of harmful bacteria from their source to humans, usually by human touch or contaminated materials. For example, a nurse’s hands become contaminated by picking up germs present on medical equipment, and they then transfer these germs to the patient if proper hand hygiene is not observed first.
The standard infection prevention and control measures in care environments are:
- Handwashing
- Use of Personal Protective Equipment (PPE)
- Washing soiled linen
- Cleaning equipment and the surrounding environment
- Safely disposing of used sharps
- Effective waste management
2.How can infections spread in hospitals?
2.a People
Patients may carry infection and can spread it by coughing and touching work surfaces. Sometimes patients may be quarantined or placed in isolation wards to minimise the spread of serious infection.
Visitors may bring contagious viruses like the common cold, or even worse Covid-19 into hospitals, where it can then spread around the wards.
2.b Different types of hospital infections
Hospital-acquired infections (HAIs) are defined as infections that occur no less than 48 hours after admission. They tend to be highest in ICUs (Intensive Care Units) where patient immunity is low.
The most prolific hospital infections are urinary tract infections (UTIs), surgical site infections (SSIs), gastroenteritis, pneumonia and sepsis.
SSIs are the most common, accounting for 16% of all infections.
2.c Effect of Covid-19
Hospital-acquired infections (HAIs) have increased during the pandemic, coinciding with periods of high hospitalisation (the first and third quarters of 2021).
Conversely though, there has been a marked decline in C. diff infections due to increased handwashing.
Ventilator-linked infections rose the most, due to the high demand for ventilators in treating Covid.
3.How do hospitals prevent the spread of infection?
3.a Standard infection control procedures
Medical staff in hospitals can improve infection control by:
- Wearing disposable gowns
- Washing hands regularly
- Following all infection control standards to prevent cross-contamination
3.b Infection Prevention and Control Team
There is a dedicated team for Infection Prevention and Control within the hospital structure. Their job is to ensure that all measures are taken to reduce and prevent healthcare-associated infections. Members of this team include physicians, nursing staff and microbiologists. Some of the ways in which they carry out their role include:
- Increasing awareness with signs
- Imposing testing requirements and handwashing rules
- Carrying out hygiene checks and audits
- Producing guidelines for all staff to follow
- Ensuring infection control is integrated into all purchasing and planning activities, for instance, when buying new equipment such as hospital chairs
3.c Statistical Outcomes
The British Medical Journal (BMJ) reported 653,000 healthcare-associated infections (HCAIs) out of 13.8 million adult inpatients in NHS England hospitals in 2016/2017.‚ 22,800 patients died as a result of their infection.
It is not just patients at risk, doctors and nurses are too. In the same year there were an additional 13,900 HCAIs among 810,000 front-line workers.
Current statistics show that 1 in every 31 hospital patients has at least one healthcare-associated infection (HCAI).ƒ
In percentage terms this is a reduction from 2016/2017 so clearly some progress has been made in the right direction.
4.Infection control in other care environments
4.a Infection control in care homes
The Care Quality Commission (CQC) has strict standards on cleanliness in care homes. Care home residents are in close proximity to each other and share facilities so it is important to keep the risk of infection as low as possible.
All care homes have to be registered and inspected by the CQC which is the regulatory body for the care sector. The CQC has infection control as one of their main priorities.
The Health and Social Care Act 2008 states that all healthcare settings must adhere to infection control procedures to prevent the spread of disease.
The CQC issue their judgement based on 8 criteria„:
- Visitors
- Shielding
- Admission
- Use of PPE
- Testing
- Premises
- Staffing
- Policies
For each of the 8 areas listed above, the CQC will judge whether they are assured, somewhat assured or not assured by what they have measured. The ‘somewhat assured’ judgement is used when minor issues have been identified, but no regulatory action is required.
If a care organisation has been judged to be ‘not assured’ by the infection control inspection, they are given 28 days to challenge the verdict before it is published by the inspectorate.
4.b Infection control in the community
Domiciliary care teams provide support for people in their own homes who need help to live independently.
The main infection precautions used in homecare settings are hand hygiene and the use of PPE.…
Care staff should always wash their hands when entering the home and before putting on PPE and delivering care. At the end of their shift, hands should be washed after removing PPE and before leaving the property or handling any food. Public health authorities have published posters showing the best way to wash hands.†
Disposable gloves, apron and face masks are the standard complet of PPE for carers.
4.c Infection control in hospices
Hospices provide end-of-life care for patients with terminal illnesses. It is critical to prevent infection in the hospice setting as it can have severe complications for patients who are already very weak and vulnerable.
It’s essential that family members know the right infection control protocols to keep their loved ones safe from infection in their final days.
All hospice visitors should follow these standard procedures:
- Washing of hands is essential when entering the hospice. Avoid touching your face so as not to spread bacteria.
- Ensure all vaccinations, particularly Covid ones are up to date to minimise the chance of contracting a virus and passing this onto patients.
- Remain at home if you are feeling unwell, rather than visiting someone who is vulnerable. Most hospice patients will have very weak immune systems.
- If you bring food into the hospice for someone, wash hands before and after handling food, and wipe down all work surfaces afterwards. A food thermometer is useful to check that meats are fully cooked.
5.How can specialist seating improve infection control?
5.a Specific features and benefits
Specialist seating can be a potential source of cross contamination, particularly in hospitals where seating rotates between patients. A number of factors can significantly reduce this risk:
- Fabric properties including waterproof for cleaning
- Minimal seams or recesses where bacteria can hide
- Smooth and flat surfaces that are easy to clean
- Impervious materials on outer chair surfaces that are more resistant to ingress of bacteria, e.g. vinyl.
We have included these key infection control features across our core product range to provide hospitals with peace of mind and conform with all infection control protocols.
- Magnetic backrest with smooth flat surface is easy to clean
- Removeable armrests for easy cleaning
- Removeable gel seat cover and cushion underneath
- Armrests and seat wrap remove for cleaning
- All surfaces compatible with chlorine-based cleaning solutions
- Magnetic handset easy to wipe clean
- Magnetic press studs instead of Velcro good for infection control
- Removeable armrests for easy cleaning
- Zip covers on legrest blocker, padded footrest and wings can be removed for easy cleaning
- Waterproof dartex material on contact surfaces
- Durable vinyl to exterior of chair
- All surfaces compatible with chlorine-based cleaning solutions
Prospec Hospital Chair:
- Developed in collaboration with infection control teams
- Flat metal base and backrest for easy cleaning
- Heavy duty vinyl is more hard-wearing for a hospital environment
- All surfaces compatible with chlorine-based cleaning solutions
5.b The role of fabrics in infection control
As we have already mentioned, vinyls are good for the outer surfaces of the chair as they are robust and do not easily absorb liquids or bacteria. Some vinyl ranges also have an extra antimicrobial coating.
Four-way stretch dartex or VP (Vapour Permeable) fabric is great for the inner surfaces of the chair as it provides good pressure relief being soft and stretchy but does not compromise on infection control, as it is waterproof, easy to clean and can have an antimicrobial coating.
Cleaning fluids to use on fabrics are detergent wipes or anti-bac wipes. Try to avoid using strong detergents or high-strength chlorine solutions as these will wear down the vinyl over time.
6.Other infection control measures
6.a Risk Assessments
Infection Prevention and Control have standard-issue risk assessments for managing infection risks in care environments.
A good example of a risk management methodology is the one used by Harrogate & District NHS Foundation Trust.‡
Decontamination forms are also used to declare the status of equipment before shipping and repair, and therefore minimise the risk of infection spreading between locations.
6.b Decontamination Units
These are purpose-built units designed to decontaminate PPE and hospital equipment. They have designated spaces for each stage of the process with built-in cleaning machines and staff facilities, making the decontamination process as efficient as possible. They are used by hospital trusts for sterilising operating equipment such as endoscopes, or for decontaminating more general items like PPE and mattresses.ˆ
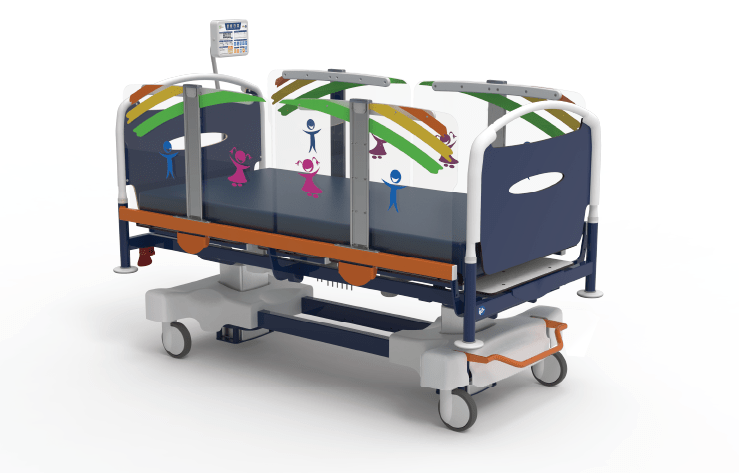
Innova Care Concepts provide a highly advanced bed washing system perfect for hospitals, using steam and robotics within a contained cleaning unit for efficient and mechanised cleaning of beds.‰
Bibliography Links
ƒ US Centers for Disease Control and Prevention (CDC): Healthcare-Associated Infections (HAIs)
„ Role of CQC in Infection Control.
†Washing hands best practice – UK Health Security Agency PDF