NHS England Push For Virtual Wards
Recently, a £200m in funding was announced for the purchase of care beds with the intention of use in ‘Virtual Wards’ & ‘Hospital at Home’ environments. This fund will allow local healthcare authorities to buy community care beds and comes on the heels of a £500m fund announced in late 2022.
With an increased recent focus on health and social care equipment in the community; we look at virtual wards (also known as hospitals at home) & their potential benefits to patients, as well as some care equipment needed for the ‘Hospital at Home’ model to run effectively.
“Up to 20% of hospital admissions can be avoided with the right care” — Health & Social Care Secretary, Steve Barclay
This push to buy care beds is part of a wider effort by NHS England that requires Integrated Care Systems (ICSs) across the UK to “deliver on virtual wards”; but what is the exact definition of a Virtual Ward?
What is a Virtual Ward?
A Virtual Ward is a safe and efficient alternative to NHS bedded care that delivers technology enabled healthcare services away from a traditional healthcare facility such as a hospital ward; often in a patient’s own home or usual place of residence including hospices and care homes.
“Virtual wards allow patients to get the care they need at home safely and conveniently, rather than being in hospital.” — NHS England
Virtual Wards can monitor a range of conditions including but not limited to:
- Osteoporosis, Frailty & Falls Recovery Treatment
- Wound Care & Pressure Injury Management
- Respiratory Illnesses & Infections
- Urinary Tract Infections (UTIs)
- Diabetes
- Oncology
- Mental health
- Learning disabilities
Patients suffering from acute respiratory infections and acute exacerbation of a frailty related conditions account for “50% of patients who may be clinically suitable to benefit from a virtual ward.”
The Virtual Ward and Hospital at Home models combine traditional health care equipment with modern technology enabled healthcare solutions to deliver patient care.
This could look like an electric care bed and moving & handling equipment in a patient’s home or place of residence; paired with a telecare service to remotely monitor patient progress.
Benefits of Virtual Wards:
There is a general perception that acute care facilities such as NHS hospitals are the safest environments for patients to recover.
This is usually the case during severe sickness; but once a patient is medical stable, recovery can be aided at home or at a patient’s regular place of residence with the correct equipment and support.
The virtual ward & hospital at home models aim to:
- Aid early discharge
- Reduce hospital admissions
- Reduce emergency department presentation
- Clear beds occupied by medically fit to discharge patients
Improving rates of hospital discharge and clearing beds in acute care facilities combined with provision of appropriate care equipment in the community means that pressure on emergency departments is eased and the time taken to complete ambulance handovers can speed up.
The Hospital at Home and Virtual Ward models look to build on the proven success of community-based virtual wards in the care of older people which can reduce emergency department (ED) presentations and reduce hospital admissions.
Virtual Wards & Hospital Acquired Infections
Virtual wards can also reduce the risk of hospital acquired infections. Along with offering a comfortable and familiar environment for a patient to recover in, a person is less at risk of hospital acquired infections when recovering in a virtual ward or hospital at home.
Sick hospital patients are likely to have reduced resistance to acquiring bacterial or fungal infections with respiratory and urinary tract infections among the most common among the most common and estimated 3.5% of these preventable HCAIs being fatal.
The most common Healthcare-associated infections (HCAIs) in NHS UK hospitals are:
- Respiratory tract infection (pneumonia etc)
- Urinary tract infections (UTIs)
- Surgical site infections (SSIs)
- Gastrointestinal infections
- Clinical sepsis
Summary:
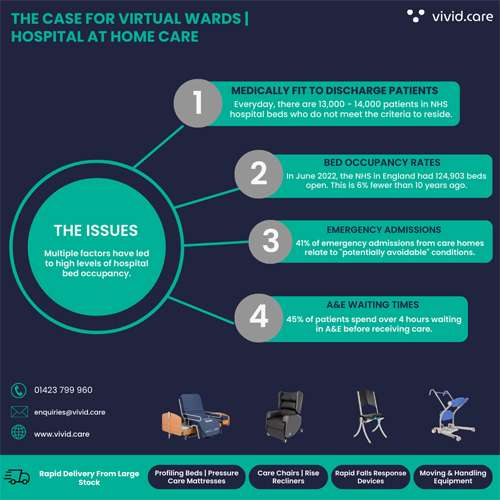
There are currently 13,000 beds occupied by patients who are “medically fit to discharge” patients who may benefit from virtual wards.
The 2022/23 NHS Priorities & Operational Planning Guidance identifies the reduction of care backlogs and patient bed days as key aims.
To help realise this target, the NHS is looking to build on the virtual wards that already exist in many areas of the UK and improve upon the 86% of Integrated Care Systems (ICSs) that have either implemented technology-enabled virtual wards or are planning to do so.
“We’re expanding care available to more people at home to reduce unnecessary trips to the hospital, help patients receive faster treatment and free up capacity in A&E.” — Steve Barclay
The ‘Virtual Ward’ and ‘Hospital at Home’ models were introduced with the goal of providing medicine, care equipment and monitoring for patients who are recovering in their own homes. The goal of these care at home services is to eventually relieve pressure on A&E departments.
More elderly and frail patients can be treated in virtual wards that will provide round-the-clock monitoring for up to 50,000 people a month with wearable tech-enabled devices that track vital signs and symptoms.
The government aims to expand the current number of Virtual Wards across the UK with plans that will see up to 10,000 extra care beds by winter 2023.